Moyamoya syndrome is a disease in which certain arteries in the brain are constricted. Blood flow is blocked by the constriction, and also by blood clots (thrombosis).
A collateral circulation develops around the blocked vessels to compensate for the blockage, but the collateral vessels are small, weak, and prone to hemorrhage, aneurysm and thrombosis. On X-rays, these collateral vessels have the appearance of a "puff of smoke" ("ã‚‚ã‚„ã‚‚ã‚„ (moyamoya)" in Japanese).
>
Etiology
The condition is believed to be hereditary and linked to q25.3, on chromosome 17 [1]. In Japan the overall incidence is higher (0.35 per 100,000). In North America, women in the third or fourth decade of life are most affected. These women frequently experience transient ischaemic attacks (TIA), cerebral hemorrhage, or may not experience any symptoms at all. They have a higher risk of recurrent stroke and may be experiencing a distinct underlying pathophysiology compared to patients from Japan.
Moyamoya can be either congenital or acquired. Patients with Down syndrome, neurofibromatosis type 1, or head trauma can develop moyamoya malformations. It is more common in women than in men, although about a third of those affected are male.
Pathophysiology
The disease Moyamoya appears to look like a "puff of smoke" because the arteries are thinned. This makes the blood leak out of the arteries, causing pressure to the brain and subsequent headaches. The pathogenesis of moyamoya disease is unknown, although the gene ring finger protein 213 (RNF213) has been implicated.
Once it begins, the process of blockage (vascular occlusion) tends to continue despite any known medical management. In some people this leads to repeated strokes and severe functional impairment or even death. In others, this blockage may not cause any symptoms.
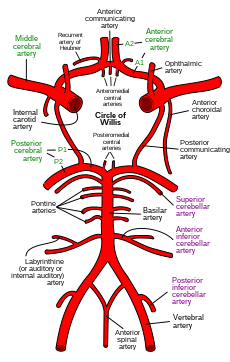
The disease causes constrictions primarily in the internal carotid artery, and often extends to the middle and anterior cerebral arteries, branches of the internal carotid artery inside the skull. When the internal carotid artery becomes completely blocked, the fine collateral circulation that it supplies is obliterated. Patients often survive on the collateral circulation from the back (posterior) of the Circle of Willis, from the basilar artery.
The constrictions of the arteries in moyamoya disease are unlike the constrictions in atherosclerosis. In atherosclerosis, the walls of arteries are damaged, leading to the deposition of fat and immune cells, and ultimately the accumulation of immune cells laden with fat. In moyamoya, the inner layer of the carotid artery proliferates within the arterial lumen. The artery also fills with blood clots, which may cause strokes.
Moyamoya is a disease that tends to affect adults in the third to fourth decade of life. In children it tends to cause strokes or seizures. In adults it tends to cause strokes or bleeding. The clinical features are strokes, recurrent transient ischemic attacks (TIAs), sensorimotor paralysis (numbness and paralysis of the extremities), convulsions and/or migraine-like headaches. Moreover, after a stroke a secondary bleed may occur. Such bleeds, called hemorrhagic strokes, may also stem from rupture of the weak neovascular vessel walls.
Diagnosis

The diagnosis of moyamoya is suggested by CT, MRI, or angiogram results. Contrast-enhanced T1-weighted images are better than FLAIR images for depicting the leptomeningeal ivy sign in moyamoya disease. MRI and MRA should be performed for the diagnosis and follow-up of moyamoya disease. Diffusion-weighted imaging can also be used for following the clinical course of children with moyamoya disease, in whom new focal deficits are highly suspicious of new infarcts.
Often nuclear medicine studies such as SPECT (single photon emission computerized tomography) are used to demonstrate the decreased blood and oxygen supply to areas of the brain involved with moyamoya disease. Conventional angiography provided the conclusive diagnosis of moyamoya disease in most cases and should be performed before any surgical considerations.
Treatment

Drugs such as antiplatelet agents (including aspirin) are usually given to prevent clots, but surgery is usually recommended. Since moyamoya tends to affect only the internal carotid artery and nearby sections of the adjacent anterior and middle cerebral arteries, surgeons can direct other arteries, such as the external carotid artery or the superficial temporal artery to replace its circulation. The arteries are either sewn directly into the brain circulation, or placed on the surface of the brain to reestablish new circulation after a few weeks.
There are many operations that have been developed for the condition, but currently the most favored are the in-direct procedures EDAS, EMS, and multiple burr holes and the direct procedure STA-MCA. Direct superficial temporal artery (STA) to middle cerebral artery (MCA) bypass is considered the treatment of choice, although its efficacy, particularly for hemorrhagic disease, remains uncertain. Multiple burr holes have been used in frontal and parietal lobes with good neovascularisation achieved.
The EDAS (encephaloduroarteriosynangiosis) procedure is a synangiosis procedure that requires dissection of a scalp artery over a course of several inches and then making a small temporary opening in the skull directly beneath the artery. The artery is then sutured to a branch of the middle cerebral artery on the surface of the brain and the bone replaced.
In the EMS (encephalomyosynangiosis) procedure, the temporalis muscle, which is in the temple region of the forehead, is dissected and through an opening in the skull placed onto the surface of the brain.
In the multiple burr holes procedure, multiple small holes (burr holes) are placed in the skull to allow for growth of new vessels into the brain from the scalp.
In the STA-MCA procedure, the scalp artery (superficial temporal artery or STA) is directly sutured to an artery on the surface of the brain (middle cerebral artery or MCA). This procedure is also commonly referred to as an EC-IC (External Carotid-Internal Carotid) bypass.
All of these operations have in common the concept of a blood and oxygen "starved" brain reaching out to grasp and develop new and more efficient means of bringing blood to the brain and bypassing the areas of blockage. The modified direct anastomosis and encephalo-myo-arterio-synagiosis play a role in this improvement by increasing cerebral blood flow (CBF) after the operation. A significant correlation is found between the postoperative effect and the stages of preoperative angiograms. It is crucial for surgery that the anesthesiologist have experience in managing children being treated for moyamoya as the type of anesthesia they require is very different from the standard anesthetic children get for almost any other type of neurosurgical procedure.
Prognosis
The natural history of this disorder is not well known. The long term outlook for patients with treated moyamoya seems to be good. While symptoms may seem to improve almost immediately after the in-direct EDAS, EMS, and multiple burr holes surgeries, it will take probably 6â€"12 months before new vessels can develop to give a sufficient blood supply. With the direct STA-MCA surgery, increased blood supply is immediate.
Once major stroke or bleeding take place, even with treatment, the patient may be left with permanent loss of function so it is very important to treat this condition promptly.
New research

Recent investigations have established that both moyamoya disease and arteriovenous fistulas (AVFs) of the lining of the brain, the dura, are associated with dural angiogenesis. These factors may represent a mechanism for ischemia contributing to the formation of dural AVFs. At least one case of simultaneous unilateral moyamoya disease and ipsilateral dural arteriovenous fistula has been reported at the Barrow Neurological Institute. In this case a 44-year-old man presented with headache, tinnitus, and an intraventricular hemorrhage, as seen on computed tomographic scans. Cerebral angiography showed a right moyamoya pattern and an ipsilateral dural AVF fed by branches of the external carotid artery and draining into the transverse sinus. This extremely rare coincidental presentation may have deeper pathogenic implications.
References

External links

- http://www.moyamoya.com
- http://www.childrenshospital.org/moyamoya
- http://moyamoya.stanford.edu
- http://www.mir.wustl.edu/research/internal.asp?NavID=707
- http://www.kispi.uzh.ch/Kinderspital/Chirurgie/Chirurgie-1/Neurochirurgie/Moyamoya_en.html
- Orphanet's disease page on Moyamoya disease







I'm 61 years old, I contracted hpv in 2011' I has be taking lot treatment for it and embarrassedsome months ago the wart stated coming out seriously, I used lot recommendation because there was lot warts around my anus and was so . but today I'm totally happy I got the virus eliminated by using natural treatment from Dr Onokun herbal center after his treatment I got cured. all the warts went away' seriously believed Dr Onokun he have the cure for human papillomavirus because he has eliminated hpv been in my body since 2011, Dr Onokun make it possible for me. Here is Dr Onokun email to reach him: Dronokunherbalcure@gmail.com he is welled capable of curing terrible diseases.
ReplyDelete