Public health is "the science and art of preventing disease, prolonging life and promoting health through the organized efforts and informed choices of society, organizations, public and private, communities and individuals." It is concerned with threats to health based on population health analysis. The population in question can be as small as a handful of people, or as large as all the inhabitants of several continents (for instance, in the case of a pandemic). The dimensions of health can encompass "a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity", as defined by the United Nations' World Health Organization. Public health incorporates the interdisciplinary approaches of epidemiology, biostatistics and health services. Environmental health, community health, behavioral health, health economics, public policy, insurance medicine and occupational safety and health are other important subfields.
The focus of public health intervention is to improve health and quality of life through the prevention and treatment of disease and other physical and mental health conditions, through surveillance of cases and health indicators, and through the promotion of healthy behaviors. Promotion of hand washing and breastfeeding, delivery of vaccinations, and distribution of condoms to control the spread of sexually transmitted diseases are examples of common public health measures.
Modern public health practice requires multidisciplinary teams of public health workers and professionals including physicians specializing in public health/community medicine/infectious disease, psychologists epidemiologists, biostatisticians, medical assistants or Assistant Medical Officers, public health nurses, midwives, medical microbiologists, environmental health officers / public health inspectors, pharmacists, dental hygienists, dietitians and nutritionists, veterinarians, public health engineers, public health lawyers, sociologists, community development workers, communications experts, bioethicists, and others.
Objectives
The focus of a public health intervention is to prevent and manage diseases, injuries and other health conditions through surveillance of cases and the promotion of healthy behaviors, communities and environments. Many diseases are preventable through simple, non-medical methods. For example, research has shown that the simple act of hand washing with soap can prevent many contagious diseases. In other cases, treating a disease or controlling a pathogen can be vital to preventing its spread to others, such as during an outbreak of infectious disease, or contamination of food or water supplies. Public health communications programs, vaccination programs, and distribution of condoms are examples of common public health measures. Measures such as these have contributed greatly to the health of populations and increases in life expectancy.
Public health plays an important role in disease prevention efforts in both the developing world and in developed countries, through local health systems and non-governmental organizations. The World Health Organization (WHO) is the international agency that coordinates and acts on global public health issues. Most countries have their own government public health agencies, sometimes known as ministries of health, to respond to domestic health issues. For example in the United States, the front line of public health initiatives are state and local health departments. The United States Public Health Service (PHS), led by the Surgeon General of the United States, and the Centers for Disease Control and Prevention, headquartered in Atlanta, are involved with several international health activities, in addition to their national duties. In Canada, the Public Health Agency of Canada is the national agency responsible for public health, emergency preparedness and response, and infectious and chronic disease control and prevention. The Public health system in India is managed by the Ministry of Health & Family Welfare of the government of India with state owned health care facilities.
There is a great disparity in access to health care and public health initiatives between developed nations and developing nations. In the developing world, public health infrastructures are still forming. There may not be enough trained health workers or monetary resources to provide even a basic level of medical care and disease prevention. As a result, a large majority of disease and mortality in the developing world results from and contributes to extreme poverty. For example, many African governments spend less than US$10 per person per year on health care, while, in the United States, the federal government spent approximately US$4,500 per capital in 2000. However, expenditures on health care should not be confused with spending on public health. Public health measures may not generally be considered "health care" in the strictest sense. For example, mandating the use of seat belts in cars can save countless lives and contribute to the health of a population, but typically money spent enforcing this rule would not count as money spent on health care.
History

Early history
Public health has early roots in antiquity. From the beginnings of human civilization, it was recognized that polluted water and lack of proper waste disposal spread communicable diseases (theory of miasma). Early religions attempted to regulate behavior that specifically related to health, from types of food eaten, to regulating certain indulgent behaviors, such as drinking alcohol or sexual relations. Leaders were responsible for the health of their subjects to ensure social stability, prosperity, and maintain order.
By Roman times, it was well understood that proper diversion of human waste was a necessary tenet of public health in urban areas. The ancient Chinese medical doctors developed the practice of variolation following a smallpox epidemic around 1000 BC. An individual without the disease could gain some measure of immunity against it by inhaling the dried crusts that formed around lesions of infected individuals. Also, children were protected by inoculating a scratch on their forearms with the pus from a lesion.
During the 14th century Black Death in Europe, it was believed that removing bodies of the dead would further prevent the spread of the bacterial infection. This did little to stem the plague, however, which was most likely spread by rodent-borne fleas. Burning parts of cities resulted in much greater benefit, since it destroyed the rodent infestations . The development of quarantine in the medieval period helped mitigate the effects of other infectious diseases.
In 1485 the Republic of Venice established a Permanent Court of supervisors of health with special attention to the prevention of the spread of epidemics in the territory from abroad. The three supervisors were initially appointed by the Venetian Senate. In 1537 it was assumed by the Grand Council, and in 1556 added two judges, with the task of control, on behalf of the Republic, the efforts of the supervisors.
However, according to Michel Foucault, the plague model of governmentality was later controverted by the cholera model. A Cholera pandemic devastated Europe between 1829 and 1851, and was first fought by the use of what Foucault called "social medicine", which focused on flux, circulation of air, location of cemeteries, etc. All those concerns, born of the miasma theory of disease, were mixed with urbanistic concerns for the management of populations, which Foucault designated as the concept of "biopower". The German conceptualized this in the Polizeiwissenschaft ("Police science").
Modern public health
The 18th century saw rapid growth in voluntary hospitals in England. The latter part of the century brought the establishment of the basic pattern of improvements in public health over the next two centuries: a social evil was identified, private philanthropists brought attention to it, and changing public opinion led to government action.
The practice of vaccination became prevalent in the 1800s, following the pioneering work of Edward Jenner in treating smallpox. James Lind's discovery of the causes of scurvy amongst sailors and its mitigation via the introduction of fruit on lengthy voyages was published in 1754 and led to the adoption of this idea by the Royal Navy. Efforts were also made to promulgate health matters to the broader public; in 1752 the British physician Sir John Pringle published Observations on the Diseases of the Army in Camp and Garrison, in which he advocated for the importance of adequate ventilation in the military barracks and the provision of latrines for the soldiers.
With the onset of the Industrial Revolution, living standards amongst the working population began to worsen, with cramped and unsanitary urban conditions. In the first four decades of the 19th century alone, London's population doubled and even greater growth rates were recorded in the new industrial towns, such as Leeds and Manchester. This rapid urbanisation exacerbated the spread of disease in the large conurbations that built up around the workhouses and factories. These settlements were cramped and primitive with no organised sanitation. Disease was inevitable and its incubation in these areas was encouraged by the poor lifestyle of the inhabitants. Unavailable housing led to the rapid growth of slums and the per capita death rate began to rise alarmingly, almost doubling in Birmingham and Liverpool. Thomas Malthus warned of the dangers of overpopulation in 1798. His ideas, as well as those of Jeremy Bentham, became very influential in government circles in the early years of the 19th century.
Public health legislation
The first attempts at sanitary reform and the establishment of public health institutions were made in the 1840s. Thomas Southwood Smith, physician at the London Fever Hospital, began to write papers on the importance of public health, and was one of the first physicians brought in to give evidence before the Poor Law Commission in the 1830s, along with Neil Arnott and James Phillips Kay. Smith advised the government on the importance of quarantine and sanitary improvement for limiting the spread of infectious diseases such as cholera and yellow fever.
The Poor Law Commission reported in 1838 that "the expenditures necessary to the adoption and maintenance of measures of prevention would ultimately amount to less than the cost of the disease now constantly engendered". It recommended the implementation of large scale government engineering projects to alleviate the conditions that allowed for the propagation of disease. The Health of Towns Association was formed in Exeter on 11 December 1844, and vigorously campaigned for the development of public health in the United Kingdom. Its formation followed the 1843 establishment of the Health of Towns Commission, chaired by Sir Edwin Chadwick, which produced a series of reports on poor and insanitary conditions in British cities.
These national and local movements led to the Public Health Act, finally passed in 1848. It aimed to improve the sanitary condition of towns and populous places in England and Wales by placing the supply of water, sewerage, drainage, cleansing and paving under a single local body with the General Board of Health as a central authority. The Act was passed by the Liberal government of Lord John Russell, in response to the urging of Edwin Chadwick. Chadwick's seminal report on The Sanitary Condition of the Labouring Population was published in 1842 and was followed up with a supplementary report a year later.
Vaccination for various diseases was made compulsory in the United Kingdom in 1851, and by 1871 legislation required a comprehensive system of registration run by appointed vaccination officers.
Further interventions were made by a series of subsequent Public Health Acts, notably the 1875 Act. Reforms included latrinization, the building of sewers, the regular collection of garbage followed by incineration or disposal in a landfill, the provision of clean water and the draining of standing water to prevent the breeding of mosquitoes. So began the inception of the modern public health.
In the U.S., the first public health organization based on a state health department and local boards of health was founded in New York City in 1866.
Epidemiology
The science of epidemiology was founded by John Snow's identification of a polluted public water well as the source of an 1854 cholera outbreak in London. Dr. Snow believed in the germ theory of disease as opposed to the prevailing miasma theory. He first publicized his theory in an essay, On the Mode of Communication of Cholera, in 1849, followed by a more detailed treatise in 1855 incorporating the results of his investigation of the role of the water supply in the Soho epidemic of 1854.
By talking to local residents (with the help of Reverend Henry Whitehead), he identified the source of the outbreak as the public water pump on Broad Street (now Broadwick Street). Although Snow's chemical and microscope examination of a water sample from the Broad Street pump did not conclusively prove its danger, his studies of the pattern of the disease were convincing enough to persuade the local council to disable the well pump by removing its handle.
Snow later used a dot map to illustrate the cluster of cholera cases around the pump. He also used statistics to illustrate the connection between the quality of the water source and cholera cases. He showed that the Southwark and Vauxhall Waterworks Company was taking water from sewage-polluted sections of the Thames and delivering the water to homes, leading to an increased incidence of cholera. Snow's study was a major event in the history of public health and geography. It is regarded as the founding event of the science of epidemiology.
Disease control
With the pioneering work in bacteriology of French chemist Louis Pasteur and German scientist Robert Koch, methods for isolating the bacteria responsible for a given disease and vaccines for remedy were developed at the turn of the 20th century. British physician Ronald Ross identified the mosquito as the carrier of malaria and laid the foundations for combating the disease. Joseph Lister revolutionized surgery by the introduction of antiseptic surgery to eliminate infection. French epidemiologist Paul-Louis Simond proved that plague was carried by fleas on the back of rats, and the Americans Walter Reed and James Carroll demonstrated that mosquitoes carry the virus responsible for yellow fever.
With onset of the epidemiological transition and as the prevalence of infectious diseases decreased through the 20th century, public health began to put more focus on chronic diseases such as cancer and heart disease. Previous efforts in many developed countries had already led to dramatic reductions in the infant mortality rate using preventative methods. In Britain, the infant mortality rate fell from over 15% in 1870 to 7% by 1930.
In the United States, public health worker Dr. Sara Josephine Baker established many programs to help the poor in New York City keep their infants healthy, leading teams of nurses into the crowded neighborhoods of Hell's Kitchen and teaching mothers how to dress, feed, and bathe their babies.
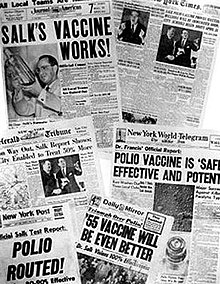
Dramatic increases in average life span in the late 19th century and 20th century, is widely credited to public health achievements, such as vaccination programs and control of many infectious diseases including polio, diphtheria, yellow fever and smallpox; effective health and safety policies such as road traffic safety and occupational safety; improved family planning; tobacco control measures; and programs designed to decrease non-communicable diseases by acting on known risk factors such as a person's background, lifestyle and environment.
Another major public health improvement was the decline in the "urban penalty" brought about by improvements in sanitation. These improvements included chlorination of drinking water, filtration and sewage treatment which led to the decline in deaths caused by infectious waterborne diseases such as cholera and intestinal diseases.
Recent
Large parts of the developing world remained plagued by largely preventable or treatable infectious diseases and poor maternal and child health, exacerbated by malnutrition and poverty. The WHO reports that a lack of exclusive breastfeeding during the first six months of life contributes to over a million avoidable child deaths each year. Intermittent preventive therapy aimed at treating and preventing malaria episodes among pregnant women and young children is one public health measure in endemic countries.
Each day brings new front-page headlines about public health: emerging infectious diseases such as SARS, rapidly making its way from China (see Public health in China) to Canada, the United States and other geographically distant countries; reducing inequities in health care access through publicly funded health insurance programs; the HIV/AIDS pandemic and its spread from certain high-risk groups to the general population in many countries, such as in South Africa; the increase of childhood obesity and the concomitant increase in type II diabetes among children; the social, economic and health effects of adolescent pregnancy; and the public health challenges related to natural disasters such as the 2004 Indian Ocean tsunami, 2005's Hurricane Katrina in the United States and the 2010 Haiti earthquake.
Since the 1980s, the growing field of population health has broadened the focus of public health from individual behaviors and risk factors to population-level issues such as inequality, poverty, and education. Modern public health is often concerned with addressing determinants of health across a population. There is a recognition that our health is affected by many factors including where we live, genetics, our income, our educational status and our social relationships; these are known as "social determinants of health." A social gradient in health runs through society. The poorest generally suffer the worst health, but even the middle classes will generally have worse health outcomes than those of a higher social stratum. The new public health advocates for population-based policies that improve health in an equitable manner.
Public Health 2.0
Public Health 2.0 is a movement within public health that aims to make the field more accessible to the general public and more user-driven. The term is used in three senses. In the first sense, "Public Health 2.0" is similar to "Health 2.0" and describes the ways in which traditional public health practitioners and institutions are reaching out (or could reach out) to the public through social media and health blogs.
In the second sense, "Public Health 2.0" describes public health research that uses data gathered from social networking sites, search engine queries, cell phones, or other technologies. In the third sense, "Public Health 2.0" is used to describe public health activities that are completely user-driven. An example is the collection and sharing of information about environmental radiation levels after the March 2011 tsunami in Japan. In all cases, Public Health 2.0 draws on ideas from Web 2.0, such as crowdsourcing, information sharing, and user-centred design.
Education and training
Education and training of public health professionals is available throughout the world in Medical Schools, Veterinary Schools, Schools of Nursing, Schools of Public Health, and Schools of Public Affairs. The training typically requires a university degree with a focus on core disciplines of biostatistics, epidemiology, health services administration, health policy, health education, behavioral science and environmental health. The National Commission for Health Education Credentialing (NCHEC) offers a national certification, Certified Health Education Specialist, C.H.E.S., for those who meet the eligibility requirements.
Schools of public health
In the United States, the Welch-Rose Report of 1915 has been viewed as the basis for the critical movement in the history of the institutional schism between public health and medicine because it led to the establishment of schools of public health supported by the Rockefeller Foundation. The report was authored by William Welch, founding dean of the Johns Hopkins Bloomberg School of Public Health, and Wycliffe Rose of the Rockefeller Foundation. The report focused more on research than practical education. Some have blamed the Rockefeller Foundation's 1916 decision to support the establishment of schools of public health for creating the schism between public health and medicine and legitimizing the rift between medicine's laboratory investigation of the mechanisms of disease and public health's nonclinical concern with environmental and social influences on health and wellness.
Even though schools of public health had already been established in Canada, Europe and North Africa, the United States had still maintained the traditional system of housing faculties of public health within their medical institutions. A $25,000 donation from businessman Samuel Zemurray instituted the School of Public Health and Tropical Medicine at Tulane University in 1912 conferring its first doctor of public health degree in 1914. The Johns Hopkins School of Hygiene and Public Health became the an independent, degree-granting institution for research and training in public health, and the largest public health training facility in the United States, when it was founded in 1916. By 1922, schools of public health were established at Columbia, Harvard and Yale on the Hopkins model. By 1999 there were twenty nine schools of public health in the US, enrolling around fifteen thousand students.
Over the years, the types of students and training provided have also changed. In the beginning, students who enrolled in public health schools typically had already obtained a medical degree; public health school training was largely a second degree for medical professionals. However, in 1978, 69% of American students enrolled in public health schools had only a bachelor's degree.
Degrees in public health
Schools of public health offer a variety of degrees which generally fall into two categories: professional or academic. The two major postgraduate degrees are the Master of Public Health (M.P.H.) or the Master of Science in Public Health (MSPH). Doctoral studies in this field include Doctor of Public Health (DrPH) and Doctor of Philosophy (Ph.D.) in a subspeciality of greater Public Health disciplines. DrPH is regarded as a professional leadership degree and Ph.D. as more of an academic degree.
Professional degrees are oriented towards practice in public health settings. The Master of Public Health, Doctor of Public Health, Doctor of Health Science (DHSc) and the Master of Health Care Administration are examples of degrees which are geared towards people who want careers as practitioners of public health in health departments, managed care and community-based organizations, hospitals and consulting firms among others. Master of Public Health degrees broadly fall into two categories, those that put more emphasis on an understanding of epidemiology and statistics as the scientific basis of public health practice and those that include a more eclectic range of methodologies. A Master of Science of Public Health is similar to an MPH but is considered an academic degree (as opposed to a professional degree) and places more emphasis on quantitative methods and research. The same distinction can be made between the DrPH and the DHSc. The DrPH is considered a professional degree and the DHSc is an academic degree.
Academic degrees are more oriented towards those with interests in the scientific basis of public health and preventive medicine who wish to pursue careers in research, university teaching in graduate programs, policy analysis and development, and other high-level public health positions. Examples of academic degrees are the Master of Science, Doctor of Philosophy, Doctor of Science (ScD), and Doctor of Health Science (DHSc). The doctoral programs are distinct from the MPH and other professional programs by the addition of advanced coursework and the nature and scope of a dissertation research project.
In the United States, the Association of Schools of Public Health represents Council on Education for Public Health (CEPH) accredited schools of public health. Delta Omega is the honor society for graduate studies in public health. The society was founded in 1924 at the Johns Hopkins School of Hygiene and Public Health. Currently, there are approximately 68 chapters throughout the United States and Puerto Rico.
Public health programs
Today, most governments recognize the importance of public health programs in reducing the incidence of disease, disability, and the effects of aging and other physical and mental health conditions, although public health generally receives significantly less government funding compared with medicine. In recent years, public health programs providing vaccinations have made strides in promoting health, including the eradication of smallpox, a disease that plagued humanity for thousands of years.
The World Health Organization (WHO) identifies core functions of public health programs including:
- providing leadership on matters critical to health and engaging in partnerships where joint action is needed;
- shaping a research agenda and stimulating the generation, translation and dissemination of valuable knowledge;
- setting norms and standards and promoting and monitoring their implementation;
- articulating ethical and evidence-based policy options;
- monitoring the health situation and assessing health trends.
In particular, public health surveillance programs can:
- serve as an early warning system for impending public health emergencies;
- document the impact of an intervention, or track progress towards specified goals; and
- monitor and clarify the epidemiology of health problems, allow priorities to be set, and inform health policy and strategies.
- diagnose, investigate, and monitor health problems and health hazards of the community
Public health surveillance has led to the identification and prioritization of many public health issues facing the world today, including HIV/AIDS, diabetes, waterborne diseases, zoonotic diseases, and antibiotic resistance leading to the reemergence of infectious diseases such as tuberculosis. Antibiotic resistance, also known as drug resistance, was the theme of World Health Day 2011. Although the prioritization of pressing public health issues is important, Laurie Garrett argues that there are following consequences. When foreign aid is funneled into disease-specific programs, the importance of public health in general is disregarded. This public health problem of stovepiping is thought to create a lack of funds to combat other existing diseases in a given country.
For example, the WHO reports that at least 220 million people worldwide suffer from diabetes. Its incidence is increasing rapidly, and it is projected that the number of diabetes deaths will double by the year 2030. In a June 2010 editorial in the medical journal The Lancet, the authors opined that "The fact that type 2 diabetes, a largely preventable disorder, has reached epidemic proportion is a public health humiliation." The risk of type 2 diabetes is closely linked with the growing problem of obesity. The WHO’s latest estimates highlighted that globally approximately 1.5 billion adults were overweight in 2008, and nearly 43 million children under the age of five were overweight in 2010. The United States is the leading country with 30.6% of its population being obese. Mexico follows behind with 24.2% and the United Kingdom with 23%. Once considered a problem in high-income countries, it is now on the rise in low-income countries, especially in urban settings. Many public health programs are increasingly dedicating attention and resources to the issue of obesity, with objectives to address the underlying causes including healthy diet and physical exercise.
Some programs and policies associated with public health promotion and prevention can be controversial. One such example is programs focusing on the prevention of HIV transmission through safe sex campaigns and needle-exchange programmes. Another is the control of tobacco smoking. Changing smoking behavior requires long-term strategies, unlike the fight against communicable diseases, which usually takes a shorter period for effects to be observed. Many nations have implemented major initiatives to cut smoking, such as increased taxation and bans on smoking in some or all public places. Proponents argue by presenting evidence that smoking is one of the major killers, and that therefore governments have a duty to reduce the death rate, both through limiting passive (second-hand) smoking and by providing fewer opportunities for people to smoke. Opponents say that this undermines individual freedom and personal responsibility, and worry that the state may be emboldened to remove more and more choice in the name of better population health overall.
Simultaneously, while communicable diseases have historically ranged uppermost as a global health priority, non-communicable diseases and the underlying behavior-related risk factors have been at the bottom. This is changing however, as illustrated by the United Nations hosting its first General Assembly Special Summit on the issue of non-communicable diseases in September 2011.
Many health problems are due to maladaptive personal behaviors. From an evolutionary psychology perspective, over consumption of novel substances that are harmful is due to the activation of an evolved reward system for substances such as drugs, tobacco, alcohol, refined salt, fat, and carbohydrates. New technologies such as modern transportation also cause reduced physical activity. Research has found that behavior is more effectively changed by taking evolutionary motivations into consideration instead of only presenting information about health effects. Thus, the increased use of soap and hand-washing to prevent diarrhea is much more effectively promoted if its lack of use is associated with the emotion of disgust. Disgust is an evolved system for avoiding contact with substances that spread infectious diseases. Examples might include films that show how fecal matter contaminates food. The marketing industry has long known the importance of associating products with high status and attractiveness to others. Conversely, it has been argued that emphasizing the harmful and undesirable effects of tobacco smoking on other persons and imposing smoking bans in public places have been particularly effective in reducing tobacco smoking.
Applications in health care
As well as seeking to improve population health through the implementation of specific population-level interventions, public health contributes to medical care by identifying and assessing population needs for health care services, including:
- Assessing current services and evaluating whether they are meeting the objectives of the health care system
- Ascertaining requirements as expressed by health professionals, the public and other stakeholders
- Identifying the most appropriate interventions
- Considering the effect on resources for proposed interventions and assessing their cost-effectiveness
- Supporting decision making in health care and planning health services including any necessary changes.
- Informing, educating, and empowering people about health issues
Implementing effective improvement strategies
To improve public health, one important strategy is to promote modern medicine and scientific neutrality to drive the public health policy and campaign, which is recommended by Armanda Solorzana, through a case study of the Rockefeller Foundation's hookworm campaign in Mexico in the 1920s. Soloranza argues that public health policy can't concern only politics or economics. Political concerns can lead government officials to hide the real numbers of people affected by disease in their regions, such as upcoming elections. Therefore, scientific neutrality in making public health policy is critical; it can ensure treatment needs are met regardless of political and economic conditions.
The history of public health care clearly shows the global effort to improve health care for all. However, in modern-day medicine, real, measurable change has not been clearly seen, and critics argue that this lack of improvement is due to ineffective methods that are being implemented. As argued by Paul E. Farmer, structural interventions could possibly have a large impact, and yet there are numerous problems as to why this strategy has yet to be incorporated into the health system. One of the main reasons that he suggests could be the fact that physicians are not properly trained to carry out structural interventions, meaning that the ground level health care professionals cannot implement these improvements. While structural interventions can not be the only area for improvement, the lack of coordination between socioeconomic factors and health care for the poor could be counterproductive, and end up causing greater inequity between the health care services received by the rich and by the poor. Unless health care is no longer treated as a commodity, global public health can ultimately not be achieved. This being the case, without changing the way in which health care is delivered to those who have less access to it, the universal goal of public health care cannot be achieved.







I'm 61 years old, I contracted hpv in 2011' I has be taking lot treatment for it and embarrassedsome months ago the wart stated coming out seriously, I used lot recommendation because there was lot warts around my anus and was so . but today I'm totally happy I got the virus eliminated by using natural treatment from Dr Onokun herbal center after his treatment I got cured. all the warts went away' seriously believed Dr Onokun he have the cure for human papillomavirus because he has eliminated hpv been in my body since 2011, Dr Onokun make it possible for me. Here is Dr Onokun email to reach him: Dronokunherbalcure@gmail.com he is welled capable of curing terrible diseases.
ReplyDeleteGood information. keep sharing.
ReplyDeleteDeep Brain Stimulation for Parkinson's in UAE