Acute lymphoblastic leukemia (ALL) or acute lymphoid leukemia is an acute form of leukemia, or cancer of the white blood cells, characterized by the overproduction of cancerous, immature white blood cellsâ€"known as lymphoblasts. In persons with ALL, lymphoblasts are overproduced in the bone marrow and continuously multiply, causing damage and death by inhibiting the production of normal cellsâ€"such as red and white blood cells and plateletsâ€"in the bone marrow and by spreading (infiltrating) to other organs. ALL is most common in childhood with a peak incidence at 2â€"5 years of age, and another peak in old age.
The symptoms of ALL are indicative of a reduced production of functional blood cells, because the leukemia wastes the resources of the bone marrow, which are normally used to produce new, functioning blood cells. These symptoms can include fever, increased risk of infection (especially bacterial infections like pneumonia, due to neutropenia; symptoms of such an infection include shortness of breath, chest pain, cough, vomiting, changes in bowel or bladder habits), increased tendency to bleed (due to thrombocytopenia) and signs indicative of anemia including pallor, tachycardia (high heart rate), fatigue and headache.
About 6,000 cases are reported in the US every year; statistics from other countries are difficult to come by, although it is known to be more common in the United States, Italy and Costa Rica. Cure is a realistic goal and is achieved in over 80% of affected children, although only 20-40% of adults can be cured. "Acute" refers to the relatively short time course of the disease to differentiate it from chronic lymphocytic leukemia, which has a potential time course of many years.
It was one of the first cancers for which an effective chemotherapeutic treatment was developed as antifolates like aminopterin and methotrexate were developed in the late 1940s by Sidney Farber and Yellapragada Subbarow. At this point in time a doctor did not need a patient's or parent's consent to try an experimental treatment on them (as the Nuremberg code had not been signed at the time) and he initially tried folic acid supplementation as a treatment for ALL, which had disastrous consequences â€" he inadvertently accelerated the deaths of these children.
Signs and symptoms
Initial symptoms are not specific to ALL, but worsen to the point that medical help is sought. They result from the lack of normal and healthy blood cells because they are crowded out by malignant and immature leukocytes (white blood cells). Therefore, people with ALL experience symptoms from malfunctioning of their erythrocytes (red blood cells), leukocytes, and platelets. Laboratory tests that might show abnormalities include blood count tests, renal function tests, electrolyte tests, and liver enzyme tests.
The signs and symptoms of ALL are variable but follow from bone marrow replacement and/or organ infiltration.
- Generalized weakness and fatigue
- Anemia
- Dizziness
- Frequent or unexplained fever and infection
- Weight loss and/or loss of appetite
- Excessive and unexplained bruising
- Bone pain, joint pain (caused by the spread of "blast" cells to the surface of the bone or into the joint from the marrow cavity)
- Breathlessness
- Enlarged lymph nodes, liver and/or spleen
- Pitting edema (swelling) in the lower limbs and/or abdomen
- Petechiae, which are tiny red spots or lines in the skin due to low platelet levels
Pathophysiology
In general, cancer is caused by damage to DNA that leads to uncontrolled cellular growth and spreads throughout the body, either by increasing chemical signals that cause growth or by interrupting chemical signals that control growth. Damage can be caused through the formation of fusion genes, as well as the dysregulation of a proto-oncogene via juxtaposition of it to the promoter of another gene, e.g. the T-cell receptor gene. This damage may be caused by environmental factors such as chemicals, drugs or radiation.
ALL is associated with exposure to radiation and chemicals in animals and humans. High level radiation exposure is a known risk factor for developing leukemia, as found by studies of survivors of atom bomb exposure in Hiroshima and Nagasaki. In animals, exposure to benzene and other chemicals can cause leukemia. Epidemiological studies have associated leukemia with workplace exposure to chemicals, but these studies are not as conclusive. Some evidence suggests that secondary leukemia can develop in individuals treated for other cancers with radiation and chemotherapy as a result of that treatment.
Diagnosis

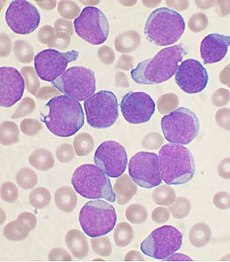
Diagnosing ALL begins with a medical history, physical examination, complete blood count, and blood smears. Because the symptoms are so general, many other diseases with similar symptoms must be excluded. Typically, the higher the white blood cell count the worse the prognosis. Blast cells are seen on blood smear in majority of cases (blast cells are precursors (stem cells) to all immune cell lines). A bone marrow biopsy is conclusive proof of ALL. A lumbar puncture (also known as a spinal tap) will tell if the spinal column and brain have been invaded.
Pathological examination, cytogenetics (in particular the presence of Philadelphia chromosome), and immunophenotyping establish whether myeloblastic (neutrophils, eosinophils, or basophils) or lymphoblastic (B lymphocytes or T lymphocytes) cells are the problem. RNA testing can establish how aggressive the disease is; different mutations have been associated with shorter or longer survival. Immunohistochemicaltesting may reveal TdT or CALLA antigens on the surface of leukemic cells. TdT is a protein expressed early in the development of pre-T and pre-B cells, whereas CALLA is an antigen found in 80% of ALL cases and also in the "blast crisis" of CML.
Medical imaging (such as ultrasound or CT scanning) can find invasion of other organs commonly the lung, liver, spleen, lymph nodes, brain, kidneys, and reproductive organs.
Cytogenetics
Cytogenetic translocations associated with specific molecular genetic abnormalities in ALL
12;21 is the most common translocation and portends a good prognosis. 4;11 is the most common in children under 12 months and portends a poor prognosis.
Classification
As ALL is not a solid tumour, the TNM notation as used in solid cancers is of little use.
FAB
Subtyping of the various forms of ALL used to be done according to the French-American-British (FAB) classification, which was used for all acute leukemias (including acute myelogenous leukemia, AML).
- ALL-L1: small uniform cells
- ALL-L2: large varied cells
- ALL-L3: large varied cells with vacuoles (bubble-like features)
Each subtype is then further classified by determining the surface markers of the abnormal lymphocytes, called immunophenotyping. There are 2 main immunologic types: pre-B cell and pre-T cell. The mature B-cell ALL (L3) is now classified as Burkitt's lymphoma/leukemia. Subtyping helps determine the prognosis and most appropriate treatment in treating ALL.
World Health Organization
The recent WHO International panel on ALL recommends that the FAB classification be abandoned, since the morphological classification has no clinical or prognostic relevance. It instead advocates the use of the immunophenotypic classification mentioned below.
- 1. Acute lymphoblastic leukemia/lymphoma. Synonyms: Former Fab L1/L2
-
- i. Precursor B acute lymphoblastic leukemia/lymphoma. Cytogenetic subtypes:
- t(12;21)(p12,q22) TEL/AML-1
- t(1;19)(q23;p13) PBX/E2A
- t(9;22)(q34;q11) ABL/BCR
- T(V,11)(V;q23) V/MLL
- ii. Precursor T acute lymphoblastic leukemia/lymphoma
- i. Precursor B acute lymphoblastic leukemia/lymphoma. Cytogenetic subtypes:
-
- 2. Burkitt's leukemia/lymphoma. Synonyms: Former FAB L3
- 3. Biphenotypic acute leukemia
Variant features
- Acute lymphoblastic leukemia with cytoplasmic granules
- Aplastic presentation of ALL
- Acute lymphoblastic leukemia with eosinophilia
- Relapse of lymphoblastic leukemia
- Secondary ALL
Immunophenotyping
The use of a TdT assay and a panel of monoclonal antibodies (MoAbs) to T cell and B cell associated antigens will identify almost all cases of ALL.
Immunophenotypic categories of acute lymphoblastic leukemia (ALL)
Treatment
The earlier acute lymphocytic leukemia is detected, the more effective the treatment. The aim is to induce a lasting remission, defined as the absence of detectable cancer cells in the body (usually less than 5% blast cells in the bone marrow).
Treatment for acute leukemia can include chemotherapy, steroids, radiation therapy, intensive combined treatments (including bone marrow or stem cell transplants), and growth factors.
Chemotherapy
Chemotherapy is the initial treatment of choice. Most ALL patients will receive a combination of different treatments. There are no surgical options, due to the body-wide distribution of the malignant cells. In general, cytotoxic chemotherapy for ALL combines multiple antileukemic drugs in various combinations. Chemotherapy for ALL consists of three phases: remission induction, intensification, and maintenance therapy.
As the chemotherapy regimens can be intensive and protracted (often about 2 years in case of the GMALL UKALL, HyperCVAD or CALGB protocols; for ALL about 3 years, 2 months for males on COG protocols; 2 years, 2 months for females - longer for males, as testicles are a potential reservoir), many patients have an intravenous catheter inserted into a large vein (termed a central venous catheter or a Hickman line), or a Portacath, a cone-shaped port with a silicone nose that is surgically planted under the skin, usually near the collar bone, and the most effective product available, due to low infection risks and the long-term viability of a portacath.
Radiation therapy
Radiation therapy (or radiotherapy) is used on painful bony areas, in high disease burdens, or as part of the preparations for a bone marrow transplant (total body irradiation). Radiation in the form of whole-brain radiation is also used for central nervous system prophylaxis, to prevent recurrence of leukemia in the brain. Whole-brain prophylaxis radiation used to be a common method in treatment of children’s ALL. Recent studies showed that CNS chemotherapy provided results as favorable but with less developmental side-effects. As a result, the use of whole-brain radiation has been more limited. Most specialists in adult leukemia have abandoned the use of radiation therapy for CNS prophylaxis, instead using intrathecal chemotherapy.
Biological therapy
For some subtypes of relapsed ALL, aiming at biological targets such as the proteasome, in combination with chemotherapy, has given promising results in clinical trials. Selection of biological targets on the basis of their combinatorial effects on the leukemic lymphoblasts can lead to clinical trials for improvement in the effects of ALL treatment. In ongoing clinical trials, a CD19-CD3 bi-specific monoclonal murine antibody - Blinatumomab, is showing great promise.
Immunotherapy
Chimeric antigen receptors (CARs) have been developed as a promising therapy for ALL. This technology uses a single chain variable fragment (scFv) designed to recognize the cell surface marker CD19 as a method of treating ALL. CD19 is a molecule found on all B-cells and can be used as a means of distinguishing the potentially malignant B-cell population in the patient. In this therapy, mice are immunized with the CD19 antigen and produce anti-CD19 antibodies. Hybridomas developed from the mouse spleen cells fused to a myeloma cell line can be developed as a source for the cDNA encoding the CD19 specific antibody. The cDNA is sequenced and the sequence encoding the variable heavy and variable light chains of these antibodies are cloned together using a small peptide linker. This resulting sequence encodes the scFv. This can be cloned into a transgene encoding what will become the endodomain of the CAR. There are varying arrangements of subunits used as the endodomain but they generally consist of the hinge region that attaches to the scFv, a transmembrane region, the intracellular region of a costimulatory molecule such as CD28, and the intracellular domain of CD3-zeta containing ITAM repeats. Other sequences frequently included are: 4-1bb and OX40. The final transgene sequence, containing the scFv and endodomain sequences is then inserted into immune effector cells that are obtained from the patient and expanded in vitro. In previous trials these have been a type of T-cell capable of cytotoxicity. Inserting the DNA into the effector cell can be accomplished by several methods. Most commonly, this is done using a lentivirus which encodes the transgene. Pseudotyped, self-inactivating lentiviruses have been shown to be an effective method for the stable insertion of a desired transgene into the target cell genomic DNA. Other methods include electroporation and transfection but these are limited in their efficacy as transgene expression will diminish over time. The gene-modified effector cells are then transplanted back into the patient. Typically this process is done in conjunction with a conditioning regiment such as cyclophosphamide which has been shown to potentiate the effects of infused T-cells. This effect has been attributed to the creation of an immunologic space niche. The process as a whole results in an effector cell, typically a T-cell, that can recognize a tumor cell antigen in a major histocompatibility complex independent manner and initiate a cytotoxic response
Prognosis
The 5-year survival rate has improved from zero six decades ago, to 85% currently, largely due to clinical trials on new chemotherapeutic agents and improvements in stem cell transplantation (SCT) technology.
Five-year survival rates evaluate older, not current, treatments. New drugs, and matching treatment to the genetic characteristics of the blast cells, may improve those rates. The prognosis for ALL differs between individuals depending on a variety of factors:
- Gender: females tend to fare better than males.
- Ethnicity: Caucasians are more likely to develop acute leukemia than African-Americans, Asians or Hispanics. However, they also tend to have a better prognosis than non-Caucasians.
- Age at diagnosis: children between 1â€"10 years of age are most likely to develop ALL and to be cured of it. Cases in older patients are more likely to result from chromosomal abnormalities (e.g., the Philadelphia chromosome) that make treatment more difficult and prognoses poorer.
- White blood cell count at diagnosis of less than 50,000/µl
- Cancer spread into the Central nervous system (brain or spinal cord) has worse outcomes.
- Morphological, immunological, and genetic subtypes
- Patient's response to initial treatment
- Genetic disorders such as Down's Syndrome
Cytogenetics, the study of characteristic large changes in the chromosomes of cancer cells, is an important predictor of outcome.
Some cytogenetic subtypes have a worse prognosis than others. These include:
- A translocation between chromosomes 9 and 22, known as the Philadelphia chromosome, occurs in about 20% of adult and 5% in pediatric cases of ALL.
- A translocation between chromosomes 4 and 11 occurs in about 4% of cases and is most common in infants under 12 months.
- Not all translocations of chromosomes carry a poorer prognosis. Some translocations are relatively favorable. For example, Hyperdiploidy (>50 chromosomes) is a good prognostic factor.
- Genome-wide copy number changes can be assessed by conventional cytogenetics or virtual karyotyping. SNP array virtual karyotyping can detect copy number changes and LOH status, while arrayCGH can detect only copy number changes. Copy neutral LOH (acquired uniparental disomy) has been reported at key loci in ALL, such as CDKN2A gene, which have prognostic significance. SNP arrayvirtual karyotyping can readily detect copy neutral LOH. Array CGH, FISH, and conventional cytogenetics cannot detect copy neutral LOH.
Correlation of prognosis with bone marrow cytogenetic finding in acute lymphoblastic leukemia
Unclassified ALL is considered to have an intermediate prognosis.
Epidemiology
US
In the US, the incidence of ALL is roughly 3000-3500 or approximately 1 in 50,000. ALL is slightly more common in males than females. In the United States in 2010, incidence in ages birth to 19 was 38.4 per 1,000,000 per year in boys and 30.2 per 1,000,000 per year in girls. Prevalence was 30,171, and observed survival was 90% (based on data from 2003-2009). ALL has a bimodal age distribution, having a high incidence in ages 2â€"5 and another peak in incidence above 50 years old. There is an increased incidence in people with Down Syndrome, Fanconi anemia, Bloom syndrome, Ataxia telangiectasia, X-linked agammaglobulinemia, and Severe combined immunodeficiency. There is an increased risk in people with a family history of autoimmune diseases, particularly autoimmune thyroid diseases (namely Graves' disease or Hashimoto's thyroiditis).
UK
ALL accounts for 8% of all leukaemia cases in the UK, and around 650 people were diagnosed with the disease in 2011.
Pregnancy
Leukemia is rarely associated with pregnancy, affecting only about 1 in 10,000 pregnant women. How it is handled depends primarily on the type of leukemia. Acute leukemias normally require prompt, aggressive treatment, despite significant risks of pregnancy loss and birth defects, especially if chemotherapy is given during the developmentally sensitive first trimester.
It is possible, although extremely rare, for leukemia to spread from mother to the child. This is called vertical transmission.
Additional images

References
External links
- Acute lymphoblastic leukemia at DMOZ
- Acute Lymphocytic Leukemia at American Cancer Society







ReplyDeletewhy not proper treatment for acute lymphoblastic leukemia
acute lymphoblastic leukemia
Hi everyone how are you, there is best treatment and free consultant guide about Acute Lymphoblastic Leukemia and telling about best hospital where is good proper diagnose.
ReplyDeleteReally nice and interesting post. I was looking for this kind of information and enjoyed reading this one. bqh online pharmacy
ReplyDeleteHOW I GOT CURED OF HERPES VIRUS.
ReplyDeleteHello everyone out there, i am here to give my testimony about a herbalist called Dr Imoloa. i was infected with herpes simplex virus 2 in 2013, i went to many hospitals for cure but there was no solution, so i was thinking on how i can get a solution out so that my body can be okay. one day i was in the pool side browsing and thinking of where i can get a solution. i go through many website were i saw so many testimonies about dr imoloa on how he cured them. i did not believe but i decided to give him a try, i contacted him and he prepared the herpes for me which i received through DHL courier service. i took it for two weeks after then he instructed me to go for check up, after the test i was confirmed herpes negative. am so free and happy. so, if you have problem or you are infected with any disease kindly contact him on email drimolaherbalmademedicine@gmail.com. or / whatssapp --+2347081986098.
This testimony serve as an expression of my gratitude. he also have
herbal cure for, FEVER, BODY PAIN, DIARRHOEA, MOUTH ULCER, MOUTH CANCER FATIGUE, MUSCLE ACHES, LUPUS, SKIN CANCER, PENILE CANCER, BREAST CANCER, PANCREATIC CANCER, CHRONIC KIDNEY DISEASE, VAGINAL CANCER, CERVICAL CANCER, DISEASE, JOINT PAIN, POLIO DISEASE, PARKINSON'S DISEASE, ALZHEIMER'S DISEASE, BULIMIA DISEASE, INFLAMMATORY JOINT DISEASE CYSTIC FIBROSIS, SCHIZOPHRENIA, CORNEAL ULCER, EPILEPSY, FETAL ALCOHOL SPECTRUM, LICHEN PLANUS, COLD SORE, SHINGLES, CANCER, HEPATITIS A, B. DIABETES 1/2, HIV/AIDS, CHRONIC RESPIRATORY DISEASE, CARDIOVASCULAR DISEASE, NEOPLASMS, MENTAL AND BEHAVIOURAL DISORDER, CHLAMYDIA, ZIKA VIRUS, EMPHYSEMA, TUBERCULOSIS LOW SPERM COUNT, ENZYMA, DRY COUGH, ARTHRITIS, LEUKAEMIA, LYME DISEASE, ASTHMA, IMPOTENCE, BARENESS/INFERTILITY, WEAK ERECTION, PENIS ENLARGEMENT. AND SO ON.
Hey, great blog, but I don’t understand how to add your site in my rss reader. Can you Help me please? мл
ReplyDelete