Muscular dystrophy (MD) is a group of muscle diseases that weaken the musculoskeletal system and hamper locomotion. Muscular dystrophies are characterized by progressive skeletal muscle weakness, defects in muscle proteins, and the death of muscle cells and tissue.
In the 1860s, descriptions of boys who grew progressively weaker, lost the ability to walk, and died at an early age became more prominent in medical journals. In the following decade, French neurologist Guillaume Duchenne gave a comprehensive account of thirteen boys with the most common and severe form of the disease, which now carries his nameâ€"Duchenne muscular dystrophy.
It soon became evident that the disease had more than one form. The other major forms are Becker, limb-girdle, congenital, facioscapulohumeral, myotonic, oculopharyngeal, distal, and Emery-Dreifuss muscular dystrophy. Duchenne and Becker muscular dystrophies, being caused by a mutation of a gene located on the X chromosome, predominantly affect males, although females can sometimes have severe symptoms as well. Most types of MD are multi-system disorders with manifestations in body systems including the heart, gastrointestinal system, nervous system, endocrine glands, eyes and brain.
Apart from the nine major types of muscular dystrophy listed above, several MD-like conditions have also been identified. Normal intellectual, muscular, behavioral, bowel and sexual function is noticed in individuals with other forms of MD and MD-like conditions. MD-affected individuals with susceptible intellectual impairment are diagnosed through molecular characteristics but not through problems associated with disability. However, a third of patients who are severely affected with DMD may have cognitive impairment, behavioral, vision and speech problems.
Signs and symptoms

- Progressive muscular wasting
- Poor balance
- Drooping eyelids
- Atrophy
- Scoliosis (curvature of the spine and the back)
- Inability to walk
- Frequent falls
- Waddling gait
- Calf deformation
- Limited range of movement
- Respiratory difficulty
- Joint contractures
- Cardiomyopathy
- Arrhythmias
- Muscle spasms
- Gowers' sign
Cause
These conditions are generally inherited, and the different muscular dystrophies follow various inheritance patterns. However, mutations of the dystrophin gene and nutritional defects (with no genetics history) at the prenatal stage are also possible in about 33% of people affected by DMD. The main cause of the Duchenne and Becker types of muscular dystrophy is the muscle tissue's cytoskeletal impairment to properly create the functional protein dystrophin and dystrophin-associated protein complex.
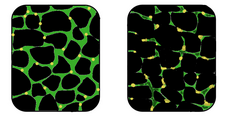
Dystrophin protein is found in muscle fibre membrane; its helical nature allows it to act like a spring or shock absorber. Dystrophin links actin (cytoskeleton) and dystroglycans of the muscle cell plasma membrane, known as the sarcolemma (extracellular). In addition to mechanical stabilization, dystrophin also regulates calcium levels.. Recent studies on the interaction of proteins with missense mutations and its neighbors showed high degree of rigidity associated with central hub proteins involved in protein binding and flexible subnetworks having molecular functions involved with calcium.
Diagnosis
The diagnosis of muscular dystrophy is based on the results of muscle biopsy, increased creatine phosphokinase (CpK3), electromyography, electrocardiography and DNA analysis.
A physical examination and the patient's medical history will help the doctor determine the type of muscular dystrophy. Specific muscle groups are affected by different types of muscular dystrophy.
Often, there is a loss of muscle mass (wasting), which may be hard to see because some types of muscular dystrophy cause a buildup of fat and connective tissue that makes the muscle appear larger. This is called pseudohypertrophy.
Management

There is no known cure for muscular dystrophy, although significant headway is being made with antisense oligonucleotides. Physical therapy, occupational therapy, orthotic intervention (e.g., ankle-foot orthosis), speech therapy and orthopedic instruments (e.g., wheelchairs, standing frames and powered mobile arm supports) may be helpful. Inactivity (such as bed rest, sitting for long periods) and bodybuilding efforts to increase myofibrillar hypertrophy can worsen the disease.
There is no specific treatment for any of the forms of muscular dystrophy. Physiotherapy, aerobic exercise, low intensity anabolic steroids, prednisone supplements may help to prevent contractures and maintain muscle tone. Orthoses (orthopedic appliances used for support) and corrective orthopedic surgery may be needed to improve the quality of life in some cases. The cardiac problems that occur with Emery-Dreifuss muscular dystrophy and myotonic muscular dystrophy may require a pacemaker. The myotonia (delayed relaxation of a muscle after a strong contraction) occurring in myotonic muscular dystrophy may be treated with medications such as quinine, phenytoin, or mexiletine, but no actual long term treatment has been found.
Occupational therapy assists the individual with MD to engage in activities of daily living (such as self-feeding and self-care activities) and leisure activities at the most independent level possible. This may be achieved with use of adaptive equipment or the use of energy conservation techniques. Occupational therapy may implement changes to a person's environment, both at home or work, to increase the individual's function and accessibility. Occupational therapists also address psychosocial changes and cognitive decline which may accompany MD, as well as provide support and education about the disease to the family and individual.
High dietary intake of lean meat, seafood, pulses, olive oil, antioxidants such as leafy vegetables and bell peppers, and fruits like blueberry and cherry is advised. Decreased intake of refined food, trans fats, and caffeinated and alcoholic beverages is also advised, as is a check for any food allergies.
After diagnosis, medical care may include services in neurology, nutrition, gastroenterology, respiratory care, cardiac care, orthopedics, psychosocial, rehabilitation, and oral care.
Prognosis

Prognosis depends on the individual form of muscular dystrophy. In some cases a person with a muscle disease will get progressively weaker to the extent that it shortens life span due to heart and breathing complications. However, some of the muscle diseases do not affect life expectancy at all. There is a tremendous amount of ongoing research to find cures and treatments to slow muscle weakness. There is also a lot of research to learn how best to manage the breathing and heart issues which generally impact lifespan more than the muscle weakness.
Types

Research funding

Within the United States, the three primary federally funded organizations that focus on muscular dystrophy research, including gene therapy, regenerative medicine) etc., include the National Institute of Neurological Disorders and Stroke (NINDS), National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), and National Institute of Child Health and Human Development (NICHD).
In 1966, the Muscular Dystrophy Association began its annual Jerry Lewis MDA Telethon, which has probably done more to raise awareness of muscular dystrophy than any other event or initiative. Disability rights advocates, however, have criticized the Jerry Lewis Telethon for portraying victims of the disease as deserving pity rather than respect.
On December 18, 2001, the MD CARE Act was signed into law and amends the Public Health Service Act to provide research for the various muscular dystrophies. This law also established the Muscular Dystrophy Coordinating Committee to help focus research efforts through a coherent research strategy.








0 comments:
Post a Comment