Melanoma (/ËŒmÉ›ləˈnoÊŠmÉ™/; from Greek μÎλας melas, "dark") is a type of skin cancer which forms from melanocytes (pigment-containing cells in the skin).
In women, the most common site is the legs, and melanomas in men are most common on the back. It is particularly common among Caucasians, especially northern Europeans and northwestern Europeans, living in sunny climates. There are higher rates in Oceania, North America, Europe, Southern Africa, and Latin America. This geographic pattern reflects the primary cause, ultraviolet light (UV) exposure in conjunction with the amount of skin pigmentation in the population. Melanocytes produce the dark pigment, melanin, which is responsible for the color of skin. These cells predominantly occur in skin, but are also found in other parts of the body, including the bowel and the eye (see uveal melanoma). Melanoma can originate in any part of the body that contains melanocytes.
The treatment includes surgical removal of the tumor. If melanoma is found early, while it is still small and thin, and if it is completely removed, then the chance of cure is high. The likelihood that the melanoma will come back or spread depends on how deeply it has gone into the layers of the skin. For melanomas that come back or spread, treatments include chemo- and immunotherapy, or radiation therapy. Five year survival rates in the United States are on average 91%.
Melanoma is less common than other skin cancers. However, it is much more dangerous if it is not found in the early stages. It causes the majority (75%) of deaths related to skin cancer. Globally, in 2012, melanoma occurred in 232,000 people and resulted in 55,000 deaths. Australia and New Zealand have the highest rates of melanoma in the world. It has become more common in the last 20 years in areas that are mostly Caucasian.
Signs and symptoms

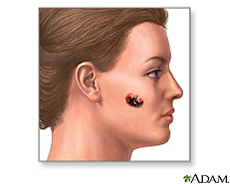
Early signs of melanoma are changes to the shape or color of existing moles or, in the case of nodular melanoma, the appearance of a new lump anywhere on the skin (such lesions should be referred without delay to a dermatologist). At later stages, the mole may itch, ulcerate or bleed. Early signs of melanoma are summarized by the mnemonic "ABCDE":
- Asymmetry
- Borders (irregular)
- Color (variegated)
- Diameter (greater than 6Â mm (0.24Â in), about the size of a pencil eraser)
- Evolving over time
These classifications do not, however, apply to the most dangerous form of melanoma, nodular melanoma, which has its own classifications:
- Elevated above the skin surface
- Firm to the touch
- Growing
Metastatic melanoma may cause nonspecific paraneoplastic symptoms, including loss of appetite, nausea, vomiting and fatigue. Metastasis of early melanoma is possible, but relatively rare: less than a fifth of melanomas diagnosed early become metastatic. Brain metastases are particularly common in patients with metastatic melanoma. It can also spread to the liver, bones, abdomen or distant lymph nodes.
Cause

Melanomas are usually caused by DNA damage resulting from exposure to ultraviolet (UV) light from the sun.
UV radiation
The UV radiation from tanning beds increases the risk of melanoma. The International Agency for Research on Cancer finds that tanning beds are "carcinogenic to humans" and that people who begin using tanning devices before age 30 are 75% more likely to develop melanoma.
Those who work in airplanes also appear to have an increase risk, believed to be due to greater exposure to UV.
Ultraviolet UVB light (wavelengths between 315 â€" 280 nm) from the sun is absorbed by skin cell DNA and results in a type of direct DNA damage called cyclobutane pyrimidine dimers (CPDs), i.e. thymine-thymine, cytosine-cytosine or cytosine-thymine dimers that are formed by the joining of two adjacent pyrimidine bases within a strand of DNA. Somewhat similarly to UVB, UVA light (longer wavelengths between 400 â€" 315 nm) from the sun or from tanning beds can also be directly absorbed by skin DNA (at about 100 to 1000 fold lower efficiency than UVB is absorbed).
Genetics
A number of rare mutations, which often run in families, are known to greatly increase one's susceptibility to melanoma. Several different genes have been identified as increasing the risk of developing melanoma. Some rare genes have a relatively high risk of causing melanoma; some more common genes, such as a gene called MC1R that causes red hair, have a relatively lower elevated risk. Genetic testing can be used to determine whether a person has one of the currently known mutations.
One class of mutations affects the gene CDKN2A. An alternative reading frame mutation in this gene leads to the destabilization of p53, a transcription factor involved in apoptosis and in fifty percent of human cancers. Another mutation in the same gene results in a nonfunctional inhibitor of CDK4, a cyclin-dependent kinase that promotes cell division. Mutations that cause the skin condition xeroderma pigmentosum (XP) also seriously predispose one to melanoma. Scattered throughout the genome, these mutations reduce a cell's ability to repair DNA. Both CDKN2A and XP mutations are highly penetrant (meaning that the chances of a person carrying the mutation to express the phenotype is very high).
Familial melanoma is genetically heterogeneous, and loci for familial melanoma have been identified on the chromosome arms 1p, 9p and 12q. Multiple genetic events have been related to the pathogenesis (disease development) of melanoma. The multiple tumor suppressor 1 (CDKN2A/MTS1) gene encodes p16INK4a â€" a low-molecular weight protein inhibitor of cyclin-dependent protein kinases (CDKs) â€" which has been localised to the p21 region of human chromosome 9.
Other mutations confer lower risk, but are more prevalent in the population. People with mutations in the MC1R gene, for example, are two to four times more likely to develop melanoma than those with two wild-type (typical unaffected type) copies of the gene. MC1R mutations are very common; in fact, all people with red hair have a mutated copy of the gene. Mutation of the MDM2 SNP309 gene is associated with increased risk of melanoma in younger women.
Pathophysiology
The earliest stage of melanoma starts when the melanocytes begin to grow out of control. Melanocytes are found between the outer layer of the skin (the epidermis) and the next layer (the dermis). This early stage of the disease is called the radial growth phase, and the tumor is less than 1Â mm thick. Because the cancer cells have not yet reached the blood vessels lower down in the skin, it is very unlikely that this early-stage cancer will spread to other parts of the body. If the melanoma is detected at this stage, then it can usually be completely removed with surgery.
When the tumor cells start to move in a different direction â€" vertically up into the epidermis and into the papillary dermis â€" the behaviour of the cells changes dramatically.
The next step in the evolution is the invasive radial growth phase, which is a confusing term; however, it explains the next step in the process of the radial growth, when individual cells start to acquire invasive potential. This step is important â€" from this point on the melanoma is capable of spreading. The Breslow's depth of the lesion is usually less than 1 mm (0.04 in), the Clark level is usually 2.
The following step in the process is the invasive melanoma â€" the vertical growth phase (VGP). The tumor attains invasive potential, meaning it can grow into the surrounding tissue and can spread around the body through blood or lymph vessels. The tumor thickness is usually more than 1 mm (0.04 in), and the tumor involves the deeper parts of the dermis.
The host elicits an immunological reaction against the tumor (during the VGP), which is judged by the presence and activity of the tumor infiltrating lymphocytes (TILs). These cells sometimes completely destroy the primary tumor; this is called regression, which is the latest stage of the melanoma development. In certain cases, the primary tumor is completely destroyed and only the metastatic tumor is discovered. About 40% of human melanomas contain activating mutations affecting the structure of the B-Raf protein, resulting in constitutive signaling through the Raf to MAP kinase pathway.
In general, cancers are caused by damage to DNA. UVA light mainly causes thymine-thymine dimers. UVA also produces reactive oxygen species and these generate other DNA damages, primarily single strand breaks, oxidized pyrimidines and the oxidized purine 8-oxoguanine (a mutagenic DNA damage) at 1/10th, 1/10th and 1/3rd the frequencies of UVA-induced thymine-thymine dimers, respectively.
If unrepaired, CPD photoproducts can lead to mutations by inaccurate translesion synthesis during DNA replication or repair. The most frequent mutations due to inaccurate synthesis past CPDs are cytosine to thymine (C>T) or CC>TT transition mutations. These are commonly referred to as UV fingerprint mutations, as they are the most specific mutation caused by UV, being frequently found in sun-exposed skin but rarely found in internal organs. Errors in DNA repair of UV photoproducts, or inaccurate synthesis past these photoproducts, can also lead to deletions, insertions and chromosomal translocations.
The entire genomes of 25 melanomas were sequenced (not only the protein-coding regions of the genome which are just 1% of the genome). On average, there were about 80,000 mutated bases (mostly C>T transitions) and about 100 structural rearragements per melanoma genome. This is a very high frequency, compared to the low mutation frequency of about 70 new mutations in the entire genome between generations (parent to child) in humans. Among the 25 melanomas, about 6,000 protein-coding genes had missense, nonsense or splice site mutations.
Diagnosis

Visual diagnosis of melanomas is still the most common method employed by health professionals. Moles that are irregular in color or shape are often treated as candidates of melanoma. To detect melanomas (and increase survival rates), it is recommended to learn what they look like (see "ABCDE" mnemonic below), to be aware of moles and check for changes (shape, size, color, itching or bleeding) and to show any suspicious moles to a doctor with an interest and skills in skin malignancy.
A popular method for remembering the signs and symptoms of melanoma is the mnemonic "ABCDE":
- Asymmetrical skin lesion.
- Border of the lesion is irregular.
- Color: melanomas usually have multiple colors.
- Diameter: moles greater than 6Â mm are more likely to be melanomas than smaller moles.
- Enlarging: Enlarging or evolving
A weakness in this system is the diameter. Many melanomas present themselves as lesions smaller than 6Â mm in diameter; and all melanomas were malignant on day 1 of growth, which is merely a dot. An astute physician will examine all abnormal moles, including ones less than 6Â mm in diameter. Seborrheic keratosis may meet some or all of the ABCD criteria, and can lead to false alarms among laypeople and sometimes even physicians. An experienced doctor can generally distinguish seborrheic keratosis from melanoma upon examination, or with dermatoscopy.
Some advocate the system "ABCDE", with E for evolution. Certainly moles that change and evolve will be a concern. Alternatively, some refer to E as elevation. Elevation can help identify a melanoma, but lack of elevation does not mean that the lesion is not a melanoma. Most melanomas are detected in the very early stage, or in-situ stage, before they become elevated. By the time elevation is visible, they may have progressed to the more dangerous invasive stage.
Nodular melanomas do not fulfill these criteria, having their own mnemonic, "EFG":
- Elevated: the lesion is raised above the surrounding skin.
- Firm: the nodule is solid to the touch.
- Growing: the nodule is increasing in size.
A recent and novel method of melanoma detection is the "ugly duckling sign". It is simple, easy to teach, and highly effective in detecting melanoma. Simply, correlation of common characteristics of a person's skin lesion is made. Lesions which greatly deviate from the common characteristics are labeled as an "Ugly Duckling", and further professional exam is required. The "Little Red Riding Hood" sign suggests that individuals with fair skin and light-colored hair might have difficult-to-diagnose amelanotic melanomas. Extra care and caution should be rendered when examining such individuals, as they might have multiple melanomas and severely dysplastic nevi. A dermatoscope must be used to detect "ugly ducklings", as many melanomas in these individuals resemble non-melanomas or are considered to be "wolves in sheep clothing". These fair-skinned individuals often have lightly pigmented or amelanotic melanomas which will not present easy-to-observe color changes and variation in colors. The borders of these amelanotic melanomas are often indistinct, making visual identification without a dermatoscope very difficult.
Amelanotic melanomas and melanomas arising in fair-skinned individuals (see the "Little Red Riding Hood" sign) are very difficult to detect, as they fail to show many of the characteristics in the ABCD rule, break the "Ugly Duckling" sign, and are very hard to distinguish from acne scarring, insect bites, dermatofibromas, or lentigines.
Following a visual examination and a dermatoscopic exam, or in vivo diagnostic tools such as a confocal microscope, the doctor may biopsy the suspicious mole. A skin biopsy performed under local anesthesia is often required to assist in making or confirming the diagnosis and in defining the severity of the melanoma. If the mole is malignant, the mole and an area around it need excision. Elliptical excisional biopsies may remove the tumor, followed by histological analysis and Breslow scoring. Punch biopsies are contraindicated in suspected melanomas, for fear of seeding tumor cells and hastening the spread of the malignant cells.
Total body photography, which involves photographic documentation of as much body surface as possible, is often used during follow-up of high-risk patients. The technique has been reported to enable early detection and provides a cost-effective approach (being possible with the use of any digital camera), but its efficacy has been questioned due to its inability to detect macroscopic changes. The diagnosis method should be used in conjunction with (and not as a replacement for) dermoscopic imaging, with a combination of both methods appearing to give extremely high rates of detection.
Classification
Melanoma is divided into the following types:
- Lentigo maligna
- Lentigo maligna melanoma
- Superficial spreading melanoma
- Acral lentiginous melanoma
- Mucosal melanoma
- Nodular melanoma
- Polypoid melanoma
- Desmoplastic melanoma
- Amelanotic melanoma
- Soft-tissue melanoma
See also:
- Melanoma with small nevus-like cells
- Melanoma with features of a Spitz nevus
- Uveal melanoma
Laboratory
Lactate dehydrogenase (LDH) tests are often used to screen for metastases, although many patients with metastases (even end-stage) have a normal LDH; extraordinarily high LDH often indicates metastatic spread of the disease to the liver. It is common for patients diagnosed with melanoma to have chest X-rays and an LDH test, and in some cases CT, MRI, PET and/or PET/CT scans. Although controversial, sentinel lymph node biopsies and examination of the lymph nodes are also performed in patients to assess spread to the lymph nodes. A diagnosis of melanoma is supported by the presence of the S-100 protein marker. HMB-45 is a monoclonal antibody that reacts against an antigen present in melanocytic tumors such as melanomas, and stands for Human Melanoma Black. It is used in anatomic pathology as a marker for such tumors. The antibody was generated to an extract of melanoma. It reacts positively against melanocytic tumors but not other tumors, thus demonstrating specificity and sensitivity. The antibody also reacts positively against junctional nevus cells but not intradermal nevi, and against fetal melanocytes but not normal adult melanocytes. HMB-45 is nonreactive with almost all non-melanoma human malignancies, with the exception of rare tumors showing evidence of melanogenesis (e.g., pigmented schwannoma, clear cell sarcoma) or tumors associated with tuberous sclerosis complex (angiomyolipoma and lymphangiomyoma).
Staging
Further context on cancer staging is available at TNM.
Also of importance are the "Clark level" and "Breslow's depth", which refer to the microscopic depth of tumor invasion.
Melanoma stages: 5 year survival rates:
Stage 0: Melanoma in situ (Clark Level I), 99.9% survival
Stage I / II: Invasive melanoma, 89â€"95% survival
- T1a: Less than 1.0Â mm primary tumor thickness, without ulceration, and mitosis < 1/mm2
- T1b: Less than 1.0 mm primary tumor thickness, with ulceration or mitoses ≥ 1/mm2
- T2a: 1.01â€"2.0 mm primary tumor thickness, without ulceration
Stage II: High risk melanoma, 45â€"79% survival
- T2b: 1.01â€"2.0 mm primary tumor thickness, with ulceration
- T3a: 2.01â€"4.0 mm primary tumor thickness, without ulceration
- T3b: 2.01â€"4.0 mm primary tumor thickness, with ulceration
- T4a: Greater than 4.0Â mm primary tumor thickness, without ulceration
- T4b: Greater than 4.0Â mm primary tumor thickness, with ulceration
Stage III: Regional metastasis, 24â€"70% survival
- N1: Single positive lymph node
- N2: Two to three positive lymph nodes or regional skin/in-transit metastasis
- N3: Four positive lymph nodes or one lymph node and regional skin/in-transit metastases
Stage IV: Distant metastasis, 7â€"19% survival
- M1a: Distant skin metastasis, normal LDH
- M1b: Lung metastasis, normal LDH
- M1c: Other distant metastasis or any distant metastasis with elevated LDH
Based upon AJCC five-year survival from initial melanoma diagnosis with proper treatment.
Prevention
Minimizing exposure to sources of ultraviolet radiation (the sun and sunbeds), following sun protection measures and wearing sun protective clothing (long-sleeved shirts, long trousers, and broad-brimmed hats) can offer protection. In the past, use of sunscreens with a sun protection factor (SPF) rating of 50 or higher on exposed areas were recommended; as older sunscreens more effectively blocked UVA with higher SPF. Currently, newer sunscreen ingredients (avobenzone, zinc, and titanium) effectively block both UVA and UVB even at lower SPFs. However, there are questions about the ability of sunscreen to prevent melanoma. This controversy is well discussed in numerous review articles, and is rejected by most dermatologists. This correlation might be due to the confounding variable that individuals who used sunscreen to prevent burn might have a higher lifetime exposure to either UVA or UVB. See Sunscreen controversy for further references and discussions. Using artificial light for tanning was once believed to help prevent skin cancers, but it can actually lead to an increased incidence of melanomas. Even though tanning beds emit mostly UVA, which causes tanning, it by itself might be enough to induce melanomas.
A good rule of thumb for decreasing ultraviolet light exposure is to avoid the sun between the hours of 9 a.m. and 3 p.m. or avoid the sun when one's shadow is shorter than one's height. These are rough rules, however, and can vary depending on locality and individual skin cancer risk.
Almost all melanomas start with altering the color and appearance of normal-looking skin. This area may be a dark spot or an abnormal new mole. Other melanomas form from a mole or freckle that is already present in the skin. It can be difficult to distinguish between a melanoma and a normal mole. When looking for danger signs in pigmented lesions of the skin, a few simple rules are often used.
Treatment

Confirmation of the clinical diagnosis is done with a skin biopsy. This is usually followed up with a wider excision of the scar or tumor. Depending on the stage, a sentinel lymph node biopsy is done, as well, although controversy exists around trial evidence for this procedure. Treatment of advanced malignant melanoma is performed from a multidisciplinary approach.
Surgery
Excisional biopsies may remove the tumor, but further surgery is often necessary to reduce the risk of recurrence. Complete surgical excision with adequate surgical margins and assessment for the presence of detectable metastatic disease along with short- and long-term followup is standard. Often this is done by a wide local excision (WLE) with 1 to 2Â cm margins. Melanoma-in-situ and lentigo malignas are treated with narrower surgical margins, usually 0.2 to 0.5Â cm. Many surgeons consider 0.5Â cm the standard of care for standard excision of melanoma-in-situ, but 0.2Â cm margin might be acceptable for margin controlled surgery (Mohs surgery, or the double-bladed technique with margin control). The wide excision aims to reduce the rate of tumor recurrence at the site of the original lesion. This is a common pattern of treatment failure in melanoma. Considerable research has aimed to elucidate appropriate margins for excision with a general trend toward less aggressive treatment during the last decades.
Mohs surgery has been reported with cure rate as low as 77% and as high as 98.0% for melanoma-in-situ. CCPDMA and the "double scalpel" peripheral margin controlled surgery is equivalent to Mohs surgery in effectiveness on this "intra-epithelial" type of melanoma.
Melanomas that spread usually do so to the lymph nodes in the area of the tumor before spreading elsewhere. Attempts to improve survival by removing lymph nodes surgically (lymphadenectomy) were associated with many complications, but no overall survival benefit. Recently, the technique of sentinel lymph node biopsy has been developed to reduce the complications of lymph node surgery while allowing assessment of the involvement of nodes with tumor.
Biopsy of sentinel lymph nodes is a widely used procedure when treating cutaneous melanoma.
Neither sentinel lymph node biopsy nor other diagnostic tests should be performed to evaluate early, thin melanoma, including melanoma in situ, T1a melanoma or T1b melanoma ≤ 0.5mm. People with these conditions are unlikely to have the cancer spread to their lymph nodes or anywhere else and already have a 97% 5-year survival rate. Because of these things, sentinel lymph node biopsy is unnecessary health care for them. Furthermore, baseline blood tests and radiographic studies should not be performed only based on identifying this kind of melanoma, as there are more accurate tests for detecting cancer and these tests have high false-positive rates.
Sentinel lymph node biopsy is often performed, especially for T1b/T2+ tumors, mucosal tumors, ocular melanoma and tumors of the limbs. A process called lymphoscintigraphy is performed in which a radioactive tracer is injected at the tumor site to localize the sentinel node(s). Further precision is provided using a blue tracer dye, and surgery is performed to biopsy the node(s). Routine hematoxylin and eosin (H&E) and immunoperoxidase staining will be adequate to rule out node involvement. Polymerase chain reaction (PCR) tests on nodes, usually performed to test for entry into clinical trials, now demonstrate that many patients with a negative sentinel lymph node actually had a small number of positive cells in their nodes. Alternatively, a fine-needle aspiration biopsy may be performed and is often used to test masses.
If a lymph node is positive, depending on the extent of lymph node spread, a radical lymph node dissection will often be performed. If the disease is completely resected, the patient will be considered for adjuvant therapy. Excisional skin biopsy is the management of choice. Here, the suspect lesion is totally removed with an adequate (but minimal, usually 1 or 2Â mm) ellipse of surrounding skin and tissue. To avoid disruption of the local lymphatic drainage, the preferred surgical margin for the initial biopsy should be narrow (1Â mm). The biopsy should include the epidermal, dermal, and subcutaneous layers of the skin. This enables the histopathologist to determine the thickness of the melanoma by microscopic examination. This is described by Breslow's thickness (measured in millimeters). However, for large lesions, such as suspected lentigo maligna, or for lesions in surgically difficult areas (face, toes, fingers, eyelids), a small punch biopsy in representative areas will give adequate information and will not disrupt the final staging or depth determination. In no circumstances should the initial biopsy include the final surgical margin (0.5Â cm, 1.0Â cm, or 2Â cm), as a misdiagnosis can result in excessive scarring and morbidity from the procedure. A large initial excision will disrupt the local lymphatic drainage and can affect further lymphangiogram-directed lymphnode dissection. A small punch biopsy can be used at any time where for logistical and personal reasons a patient refuses more invasive excisional biopsy. Small punch biopsies are minimally invasive and heal quickly, usually without noticeable scarring.
Adjuvant treatment
High-risk melanomas may require adjuvant treatment, although attitudes to this vary in different countries. In the United States, most patients in otherwise good health will begin up to a year of high-dose interferon treatment, which has severe side effects, but may improve the patient's prognosis slightly. However British Association of Dermatologist guidelines on melanoma state that interferon is not recommended as a standard adjuvant treatment for melanoma. A 2011 meta-analysis showed that interferon could lengthen the time before a melanoma comes back but increased survival by only 3% at 5 years. The unpleasant side effects also greatly decrease quality of life.
In Europe, interferon is usually not used outside the scope of clinical trials.
Metastatic melanomas can be detected by X-rays, CT scans, MRIs, PET and PET/CTs, ultrasound, LDH testing and photoacoustic detection.
Chemotherapy and immunotherapy
Various chemotherapy agents, including dacarbazine (also termed DTIC), immunotherapy (with interleukin-2 (IL-2) or interferon (IFN)), as well as local perfusion, are used by different centers. The overall success in metastatic melanoma is quite limited. IL-2 (Proleukin) is the first new therapy approved for the treatment of metastatic melanoma in 20 years. Studies have demonstrated that IL-2 offers the possibility of a complete and long-lasting remission in this disease, although only in a small percentage of patients. As of 2005 A number of new agents and novel approaches are under evaluation and show promise. As of 2009 Clinical trial participation should be considered the standard of care for metastatic melanoma.
Other options include ipilimumab (a biological immmunotherapy agent), and chemotherapy drugs such as vemurafenib and temozolomide.
Lentigo maligna treatment
Standard excision is still being done by most surgeons. Unfortunately, the recurrence rate is exceedingly high (up to 50%). This is due to the ill-defined visible surgical margin, and the facial location of the lesions (often forcing the surgeon to use a narrow surgical margin). The narrow surgical margin used, combined with the limitation of the standard "bread-loafing" technique of fixed tissue histology â€" result in a high "false negative" error rate, and frequent recurrences. Margin control (peripheral margins) is necessary to eliminate the false negative errors. If bread loafing is used, distances from sections should approach 0.1 mm to assure that the method approaches complete margin control.
Mohs surgery has been done with cure rate reported to be as low as 77%, and as high as 95% by another author. The "double scalpel" peripheral margin controlled excision method approximates the Mohs method in margin control, but requires a pathologist intimately familiar with the complexity of managing the vertical margin on the thin peripheral sections and staining methods.
Some melanocytic nevi, and melanoma-in-situ (lentigo maligna) have resolved with an experimental treatment, imiquimod (Aldara) topical cream, an immune enhancing agent. Some dermasurgeons are combining the 2 methods: surgically excising the cancer and then treating the area with Aldara cream postoperatively for three months.
Radiation therapy
Radiation therapy is often used after surgical resection for patients with locally or regionally advanced melanoma or for patients with unresectable distant metastases. It may reduce the rate of local recurrence but does not prolong survival. Radioimmunotherapy of metastatic melanoma is currently under investigation. Radiotherapy has a role in the palliation of metastatic melanoma.
Prognosis
Features that affect prognosis are tumor thickness in millimeters (Breslow's depth), depth related to skin structures (Clark level), type of melanoma, presence of ulceration, presence of lymphatic/perineural invasion, presence of tumor-infiltrating lymphocytes (if present, prognosis is better), location of lesion, presence of satellite lesions, and presence of regional or distant metastasis. Certain types of melanoma have worse prognoses but this is explained by their thickness. Interestingly, less invasive melanomas even with lymph node metastases carry a better prognosis than deep melanomas without regional metastasis at time of staging. Local recurrences tend to behave similarly to a primary unless they are at the site of a wide local excision (as opposed to a staged excision or punch/shave excision) since these recurrences tend to indicate lymphatic invasion.
When melanomas have spread to the lymph nodes, one of the most important factors is the number of nodes with malignancy. Extent of malignancy within a node is also important; micrometastases in which malignancy is only microscopic have a more favorable prognosis than macrometastases. In some cases micrometastases may only be detected by special staining, and if malignancy is only detectable by a rarely employed test known as the polymerase chain reaction (PCR), the prognosis is better. Macrometastases in which malignancy is clinically apparent (in some cases cancer completely replaces a node) have a far worse prognosis, and if nodes are matted or if there is extracapsular extension, the prognosis is worse still.
When there is distant metastasis, the cancer is generally considered incurable. The five-year survival rate is less than 10%. The median survival is 6â€"12 months. Treatment is palliative, focusing on life extension and quality of life. In some cases, patients may live many months or even years with metastatic melanoma (depending on the aggressiveness of the treatment). Metastases to skin and lungs have a better prognosis. Metastases to brain, bone and liver are associated with a worse prognosis.
There is not enough definitive evidence to adequately stage, and thus give a prognosis for, ocular melanoma and melanoma of soft parts, or mucosal melanoma (e.g. rectal melanoma), although these tend to metastasize more easily. Even though regression may increase survival, when a melanoma has regressed, it is impossible to know its original size and thus the original tumor is often worse than a pathology report might indicate.
Epidemiology
Generally, an individual's risk for developing melanoma depends on two groups of factors: intrinsic and environmental. "Intrinsic" factors are generally an individual's family history and inherited genotype, while the most relevant environmental factor is sun exposure.
Epidemiologic studies suggest that exposure to ultraviolet radiation (UVA and UVB) is one of the major contributors to the development of melanoma. UV radiation causes damage to the DNA of cells, typically thymine dimerization, which when unrepaired can create mutations in the cell's genes. When the cell divides, these mutations are propagated to new generations of cells. If the mutations occur in protooncogenes or tumor suppressor genes, the rate of mitosis in the mutation-bearing cells can become uncontrolled, leading to the formation of a tumor. Data from patients suggest that aberrant levels of activating transcription factor in the nucleus of melanoma cells are associated with increased metastatic activity of melanoma cells; studies from mice on skin cancer tend to confirm a role for activating transcription factor-2 in cancer progression. Occasional extreme sun exposure (resulting in "sunburn") is causally related to melanoma. Melanoma is most common on the back in men and on legs in women (areas of intermittent sun exposure). The risk appears to be strongly influenced by socio-economic conditions rather than indoor versus outdoor occupations; it is more common in professional and administrative workers than unskilled workers. Other factors are mutations in or total loss of tumor suppressor genes. Use of sunbeds (with deeply penetrating UVA rays) has been linked to the development of skin cancers, including melanoma.
Possible significant elements in determining risk include the intensity and duration of sun exposure, the age at which sun exposure occurs, and the degree of skin pigmentation. Melanoma rates tend to be highest in countries settled by migrants from northern Europe that have a large amount of direct, intense sunlight that the people's skin aren't adapted to, most notably Australia. Exposure during childhood is a more important risk factor than exposure in adulthood. This is seen in migration studies in Australia where people tend to retain the risk profile of their country of birth if they migrate to Australia as an adult. Individuals with blistering or peeling sunburns (especially in the first twenty years of life) have a significantly greater risk for melanoma. This does not mean that sunburn is the cause of melanoma. Instead it is merely statistically correlated. The cause is the exaggerated UV-exposure. It has been shown that sunscreen â€" while preventing the sunburn â€" does not protect mice, injected with melanoma cells a day after UV exposure, from developing melanoma.
Fair- and red-haired people, persons with multiple atypical nevi or dysplastic nevi and persons born with giant congenital melanocytic nevi are at increased risk.
A family history of melanoma greatly increases a person's risk because mutations in CDKN2A, CDK4 and several other genes have been found in melanoma-prone families. Patients with a history of one melanoma are at increased risk of developing a second primary tumor.
The incidence of melanoma has increased in the recent years, but it is not clear to what extent changes in behavior, in the environment, or in early detection are involved.
To understand how sunscreen can reduce sunburn and at the same time cause melanoma it is necessary to distinguish between direct DNA damage and indirect DNA damage. Genetic analysis has shown that 92% of all melanoma are caused by the indirect DNA damage. Although some people believe that dark-skinned people such as those of African descent cannot get sunburns, they are in fact susceptible, and should use sunscreen accordingly, as sunscreen has been proven to protect against other cancers such as squamous cell carcinoma and basal cell carcinoma.
Australia continues to experience a very high - and increasing - burden from melanoma; in 2012, deaths from melanoma were 7.3-9.8 per 100,000 population. In Australia, melanoma is the third most common cancer in either sex; indeed, its incidence is higher than for lung cancer, although the latter accounts for more deaths. It is estimated that in 2012, more than 12,000 Australians were diagnosed with melanoma: given Australia's modest population, this is better expressed as 59.6 new cases per 100,000 population per year; >1 in 10 of all new cancer cases were melanomas Melanoma incidence in Australia is matter of significance, for the following reasons:
- Australian melanoma incidence has increased by more than 30 per cent between 1991 and 2009.
- Australian melanoma age-standardised incidence rates were, as of 2008, at least 12 times higher than the world average.
- Australian melanoma incidence is, by some margin, the highest in the world.
- Overall age-standardised cancer incidence in Australia is the highest in the world, and this is attributable to melanoma alone. Age-standardised overall cancer incidence is similar to New Zealand, but there is a statistically-significant difference between Australia and all other parts of the developed world including North America, Western Europe, and the Mediterranean.
History

Although melanoma is not a new disease, evidence for its occurrence in antiquity is rather scarce. However, one example lies in a 1960s examination of nine Peruvian mummies, radiocarbon dated to be approximately 2400 years old, which showed apparent signs of melanoma: melanotic masses in the skin and diffuse metastases to the bones.
John Hunter is reported to be the first to operate on metastatic melanoma in 1787. Although not knowing precisely what it was, he described it as a "cancerous fungous excrescence". The excised tumor was preserved in the Hunterian Museum of the Royal College of Surgeons of England. It was not until 1968 that microscopic examination of the specimen revealed it to be an example of metastatic melanoma.
The French physician René Laennec was the first to describe melanoma as a disease entity. His report was initially presented during a lecture for the Faculté de Médecine de Paris in 1804 and then published as a bulletin in 1806. The first English language report of melanoma was presented by an English general practitioner from Stourbridge, William Norris in 1820. In his later work in 1857 he remarked that there is a familial predisposition for development of melanoma (Eight Cases of Melanosis with Pathological and Therapeutical Remarks on That Disease). Norris was also a pioneer in suggesting a link between nevi and melanoma and the possibility of a relationship between melanoma and environmental exposures, by observing that most of his patients had pale complexions. He also described that melanomas could be amelanotic and later showed the metastatic nature of melanoma by observing that they can disseminate to other visceral organs.
The first formal acknowledgment of advanced melanoma as untreatable came from Samuel Cooper in 1840. He stated that the only chance for a cure depends upon the early removal of the disease (i.e., early excision of the malignant mole) ...' More than one and a half centuries later this situation remains largely unchanged.
Research
Pharmacotherapy research for unresectable or metastatic malignant melanoma offers new treatment possibilities. In addition to the advances with recently approved agents, ongoing research into combination therapy, such as dabrafenib and trametinib, may reveal a more effective and better-tolerated option for patients with metastatic melanoma. One important pathway in melanin synthesis involves the transcription factor MITF. The MITF gene is highly conserved and is found in people, mice, birds, and even fish. MITF production is regulated via a fairly straightforward pathway. UV radiation causes increased expression of transcription factor p53 in keratinocytes, and p53 causes these cells to produce melanocyte-stimulating hormone (MSH), which binds to melanocortin 1 receptors (MC1R) on melanocytes. Ligand-binding at MC1R receptors activates adenylate cyclases, which produce cAMP, which activates CREB, which promote MITF expression. The targets of MITF include p16 (a CDK inhibitor) and Bcl2, a gene essential to melanocyte survival. It is often difficult to design drugs that interfere with transcription factors, but perhaps new drugs will be discovered that can impede some reaction in the pathway upstream of MITF.
Studies of chromatin structure also promise to shed light on transcriptional regulation in melanoma cells. It has long been assumed that nucleosomes are positioned randomly on DNA, but murine studies of genes involved in melanin production now suggest that nucleosomes are stereotypically positioned on DNA. When a gene is undergoing transcription, its transcription start site is almost always nucleosome-free. When the gene is silent, however, nucleosomes often block the transcriptional start site, suggesting that nucleosome position may play a role in gene regulation.
Finally, given the fact that melanin helps protect skin cells from UV-induced damage, new melanoma prevention strategies could involve attempts to induce melanin synthesis in individuals who would otherwise get sunburns. Redheads, for example, do not tan because they have MC1R mutations. In mice, it has been shown that the melanin production pathway can be rescued downstream of MC1R.
A study published on January 27, 2011, by M. Raza Zaidi et al. shows that interferon-γ links ultraviolet radiation to melanomagenesis in mice. Using a mouse model that allowed the visual tracking and purification of melanocytes using a green fluorescent dye, data showed that UVB-induced, macrophage-enhanced interferon-γ release results in melanoma growth, proliferation and immunoevasion. Based on these results, the interferon-γ pathway can potentially serve as part of new therapeutic measures to treat patients suffering from malignant melanoma, as well as a potential preventive strategy against UV-induced radiation.
BRAF
About 60% of melanomas contain a mutation in the B-Raf gene. Early clinical trials suggested that B-Raf inhibitors including Plexxicon's vemurafenib could lead to substantial tumor regression in a majority of patients if their tumor contain the B-Raf mutation. In June 2011, a large clinical trial confirmed the positive findings from those earlier trials.
In June 2012 a study reported that patients taking a different B-Raf inhibitor, Dabrafenib, did better than patients taking a chemotherapy agent.
Some researchers believe that combination therapies that simultaneously block multiple pathways may improve efficacy by making it more difficult for the tumor cells to mutate before being destroyed. In October 2012 a study reported that combining Dabrafenib with a MEK inhibitor trametinib led to even better outcomes. Compared to Dabrafenib alone, progression-free survival was increased to 41% from 9%, and the median progression-free survival increased to 9.4 months versus 5.8 months. Some side effects were, however, increased in the combined study.
Ipilimumab
At the American Society of Clinical Oncology Conference in June 2010, the Bristol-Myers Squibb pharmaceutical company reported the clinical findings of their drug ipilimumab. The study found an increase in median survival from 6.4 to 10 months in patients with advanced melanomas treated with the monoclonal ipilimumab, versus an experimental vaccine. It also found a one year survival rate of 25% in the control group using the vaccine, 44% in the vaccine and ipilimumab group, and 46% in the group treated with ipilimumab alone. However, some have raised concerns about this study for its use of the unconventional control arm, rather than comparing the drug against a placebo or standard treatment. The criticism was that although Ipilimumab performed better than the vaccine, the vaccine has not been tested before and may be causing toxicity, making the drug appear better by comparison.
Ipilimumab was approved by the FDA in March 2011 to treat patients with late-stage melanoma that has spread or cannot be removed by surgery.
In June 2011, a clinical trial of ipilimumab plus dacarbazine combined this immune system booster with the standard chemotherapy drug that targets cell division. It showed an increase in median survival for these late stage patients to 11 months instead of the 9 months normally seen. Researchers were also hopeful that perhaps 10â€"20% of patients could live a long time. Some serious side-effects of revving up the immune system were seen in some patients. A course of treatment costs $120,000. The drug's brandname is Yervoy.
Targeted therapies
In clinical research setting other therapies, such as adoptive cell therapy or gene therapy, may be tested. Two kinds of experimental treatments developed at the National Cancer Institute (NCI), part of the National Institutes of Health (NIH) in the US, have been used in advanced (metastatic) melanoma with high success rates in terms of melanoma treatments. The first treatment involves adoptive cell therapy (ACT) using TILs immune cells (tumor infiltrating lymphocytes) isolated from a patient's own melanoma tumor. These cells are grown in large numbers in a laboratory and returned to the patient after a treatment that temporarily reduces normal T cells in the patient's body. TIL therapy following lymphodepletion can result in durable complete response in a variety of setups. Up to date, the only medical center outside the USA that has managed to successfully implement this technology is Sheba Medical Center through "Ella Institute of Melanoma", found in Israel (objective response rates of 50%). The second treatment, adoptive transfer of genetically altered autologous lymphocytes, depends on delivering genes that encode so called T cell receptors (TCRs), into patient's lymphocytes. After that manipulation lymphocytes recognize and bind to certain molecules found on the surface of melanoma cells and kill them.
A new treatment that trains the immune system to fight cancer has shown modest benefit in late-stage testing against melanoma. Sutent may be effective for patients with metastatic melanoma.
Surveillance methods
Advances in high resolution ultrasound scanning have enabled surveillance of metastatic burden to the sentinel lymph nodes. The Screening and Surveillance of Ultrasound in Melanoma trial (SUNMEL) is evaluating ultrasound as an alternative to invasive surgical methods.
Oncolytic virotherapy
In some countries oncolytic virotherapy methods are studied and used to treat melanoma. Oncolytic virotherapy is a promising branch of virotherapy, where oncolytic viruses are used to treat diseases; viruses can increase metabolism, reduce anti-tumor immunity and disorganize vasculature.







An upcoming Bollywood film called "Padman" aims to help remove the stigma around periods. One of the most famous actors in Bollywood Akshay Kumar, plays social activist Arunachalam Muruganantham — the lead role in the film, which is inspired by a true Watch Latest Vidoes At Pinoytvtoday.
ReplyDeleteThe Blob Another classic horror film is The Blob. Nowadays it may be reverting more to the cheesy side of horror films, but this flick certainly made its viewers jump back in the day. This story revolves around a shapeless mass that expands as it conquers each Watch HD Vidoes At Pinoytvtoday.
ReplyDeleteAn Inconvenient Truth' premiered at the 2006 Sundance Film Festival and opened in New York City and Los Angeles on May 24, 2006, it was a critical and box-office success, winning Academy Awards for Best Documentary and Best Original Watch Vidoes At Pinoytvtoday.
ReplyDeleteThis film shouts Stephen Spielberg and comes with the usual wonderful big sci-fi film in typical J.J Abrams style. Super 8 is a little different, very beautiful and the story is amazing. Released during the summer , the film is an exciting one and worth Watch Vidoes At Pinoytvtoday.
ReplyDeleteThe title of Beverly Gray's insightful look back at 1967's "The Graduate," one of the most popular comedies of all time, is a bit misleading - Mrs. Robinson seduced young Benjamin Braddock, not the generation that identified with his anxieties about the future and dreamed of joining him in rejecting the path blazed by their Watch HQ Vidoes At Pinoytvtoday.
ReplyDeleteA flurry of sexual assault allegations has occurred this year against powerful men in the US entertainment, media and political Watch HQ Vidoes At Pinoytvtoday.
ReplyDeleteI'm 61 years old, I contracted hpv in 2011' I has be taking lot treatment for it and some months ago the wart stated coming out seriously, I used lot recommendation because there was lot warts around my anus and was so embarrassed. but today I'm totally happy I got the virus eliminated by using natural treatment from Dr Onokun herbal center after his treatment I got cured. all the warts went away' seriously believed Dr Onokun he have the cure for human papillomavirus because he has eliminated hpv been in my body since 2011, Dr Onokun make it possible for me. Here is Dr Onokun email to reach him: Dronokunherbalcure@gmail.com he is welled capable of curing terrible diseases.
ReplyDeleteHappiness is all i see now I never thought that I will live on
ReplyDeleteearth before the year runs out. I have been suffering from a
deadly disease (Herpes) for the past 3 years now; I had spent
a lot of money going from one places to another, from
churches to churches, hospitals have been my home every day
residence. Constant checks up have been my hobby not until
this faithful day, I was searching through the internet, I saw a
testimony on how pp him +2348154637647 Dr Lucky, helped
someone in curing his Herpes disease, quickly I copied his
email which is (drluckyherbalcure@gmail.com) just to give
him a test I spoke to him, he asked me to do some certain
things which I did, he told me that he is going to provide the
herbal cure to me, which he did, then he asked me to go for
medical checkup after some days after using the herbal cure, I
was free from the deadly disease, he only asked me to post
the testimony through the whole world, faithfully am doing it
now, please brothers and sisters, he is great, I owe him in
return. if you are having a similar problem just email him on
(drluckyherbalcure@gmail.com) or Call him or WhatsApp him
+2348154637647
I’m here to testify about what DR. ISIBOR did for me. I have been suffering from (GENITAL HERPES VIRUS) disease for the past 3 years and had constant pain and inching, especially in my private part. During the first year, I had faith in God that i would be cured someday.This disease started circulating all over my body and I have been taking treatment from my doctor, few weeks ago I came across a testimony of Rose Smith on the internet testifying about a Man called DR. ISIBOR on how he cured her from 7 years HSV 2. And she also gave the email address of this man, advise anybody to contact him for help on any kind of diseases that he would be of help, so I emailed him telling him about my (HSV 2) he told me not to worry that I was going to be cured!! Well, I never doubted him I have faith he can cure me too,, DR. ISIBOR prepared and sent me Healing Oil, Soap, roots and herbs which I took. In the first one week, I started experiencing changes all over me, after four weeks of using his Roots/ Herbs, Oil and Soap, I was totally cured. no more inching , pain on me anymore as DR. ISIBOR assured me. After some time I went to my doctor to do another test behold the result came out negative. So friends my advise is if you have such disease or know anyone who suffers from it or any other disease like HPV, HIV, ALS, CANCER etc. you can contact DR. ISIBOR for help via email} drisiborspellhome@gmail.com or call +2348107855231
ReplyDeleteCan't still believe that i got cured from Genital Herpes through herbal treatment from Dr LUCKY who I met through the internet, I actually couldn't believe it at first because it sounded impossible to me knowing how far I have gone just to get rid of it. Dr LUCKY send me his medicine which I took as instructed and here I am living a happy life once again, a big thanks to Dr LUCKY , I am sure there are many herbal doctors out there but Dr LUCKY did it for me, contact him on Email him; { drluckyherbalcure@gmail.com }
ReplyDeleteContact DR OMOLADE to get complete herbal cure for herpes virus and other deadly disease. I use to be positive with herpes virus but am completely negative now with the help of DR OMOLADE Herbs. I got to know about DR OMOLADE and he sent me a herbal medicine that i took for 17 days and now i am completely Negative of herpes virus without any side effect or complain. Contact DR KHAM for cure to all disease and i am sure you will find complete solution with him. For more information you can contact him on his Email: dromoladeherbalcenter@gmail.com or Whatsapp: +2349077303355 for more information.
ReplyDeleteYou can Also
He can also cure the following diseases/virus,
1) HIV/AIDs Virus
2) Hepatitis B and C
3) Herpes
4) Cancer
5) ZIKA VIRUS
6) COPD
7) STROKE.
8) Erectile Dysfunction
9) Trichomoniasis
10) Chlaydia
11) Gonorrhea
12) HPV
13) Syphilis
5 years ago I had warts, I was treated with some liquid applied to the warts they continued to grow and spread... The next 2 doctors did laser surgery to remove them. 1 year after the surgery, they grew back close to where the 1st ones were' so I was finally told it was hpv. I have had it for very long time, I contract it from my cheated boyfriend and I found out he was also infected and I end up the relationship between us. the warts was so embarrasses because it started spreading all over I have be dealing with this things for very long time the last treatment I take was About 2 years ago I applied natural treatment from Dr onokun herbal cure, a week after applying the treatment all the warts was gone. it's now 2 years and some months I don't have single wart or any symptoms of hpv. wow"" it's great, Dr onokun has finally cured me. Anyone living with hpv contact Dr onokun for natural treatment.
ReplyDeleteHis email address: Dronokunherbalcure@gmail.com
herpes is a serious and recurring disease which can't be cured through drugs or injections by the American doctors but the best way to deal with herpes is by taking natural herbs medicine for it and is only few American doctors that know about this herbal medicine from Dr Akhanene .. I have read about Dr Akhanene the great herbalist doctor from African who can cure disease with his powerful herbal medicine. for the people suffering from the following diseases, Herpes, Cancer, Also,Herpatitis, Diabetes, Hps,Infections ETC should contact him for his herbal medicine because i am a living testimony and i was cured of herpes. Although, i sent him what he requested and he sent me his medicine which i took for 1 weeks and today when i went for test i was tested herpes negative. you can reach him through his Emai drakhanenespellhome@gmail.com.com or whatsapp or call him +2348168714427
ReplyDeleteIt is a very informative and useful post thanks it is good material to read this post increases my knowledge. Executive Health Check Sydney
ReplyDelete